The patient was a 72-year-old Caucasian male with a past medical history significant for hypertension, hyperlipidemia, coronary artery disease with two prior stents, more than 10 pack years of smoking history, and chronic obstructive pulmonary disease (COPD) who presented to the emergency department (ED) with 3 weeks of worsening right ear pain. The patient initially presented to his primary care physician for the ear pain and on physical exam the ear canal was tender with swelling and a limited amount of yellow-colored discharge. The tympanic membrane was not injected, scarred, perforated, or erythematous. The patient had chronic hearing loss from presbycusis bilaterally, so hearing aids were in place but had no signs of sensorineural hearing loss. Ultimately, the patient was diagnosed with acute otitis externa of his right ear and was prescribed otofloxacin ear drops. However, 5 days into his 10-day course the patient began experiencing non-bloody drainage from the right ear and swelling behind/in front of the ear. At this time the patient decided to come to the ED. Other associated symptoms included weakness, fatigue, and dyspnea on exertion that had progressed during this time. The patient did not have any changes in his baseline cough and denied fever, chills, chest pain, headache, visual changes, nasal congestion, sore throat, nausea, and vomiting. The patient also denied similar symptoms on the left side. The rest of the review of systems was unremarkable.
The patient’s vital signs upon arrival to the department indicated that he was afebrile at 98.1° Fahrenheit, normotensive with a blood pressure of 98/65 mmHg, sinus tachycardic with a heart rate of 140–150 beats per minute, respiratory rate of 24 breaths per minute, and saturating at an SPO2 of 94% on 2L nasal cannula.
Upon physical exam, the patient was an acutely ill-appearing male in mild distress owing to right ear pain. There was crusted drainage from the right ear, edema, and erythema overlying the mastoid bone, and a round tender mass with fluctuance inferior to the lateral mandible overlaying the sternocleidomastoid. A bedside ear, nose, and throat (ENT) exam showed similar tympanic membrane findings to those previously mentioned. Furthermore, the patient was tachycardic, with no murmur, and had bilateral wheezing in all fields. The extremities showed trace edema bilaterally in the lower extremities. Cranial nerves 2 through 12 were intact, and the patient showed no signs of meningismus.
His initial workup revealed leukocytosis with 31,000 cells/mcL and a high neutrophil band percentage of 11%. The complete metabolic panel (CMP) showed hyponatremia with 127 mEq/L and hyperglycemia with 166 mg/dl. It should be noted that the patient had a normal A1c (5.4) 1 month prior to this admission, so we suspected the hyperglycemia to be stress-induced. The remainder of the lab values were normal or nonpertinent to diagnosis. Methicillin-resistant Staphylococcus aureus (MRSA) nares and viral polymerase chain reaction (PCR) were also collected in the ED and were negative, and blood cultures showed no immediate results.
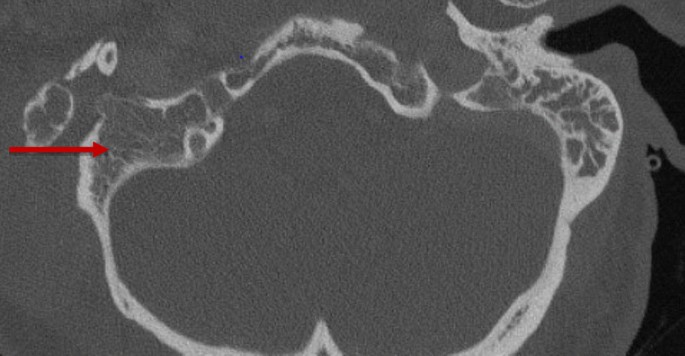
A noncontrast computed tomography (CT) scan of the temporal bones and a chest X-ray were ordered in the ED. The CT showed coalescent right acute mastoiditis with a subperiosteal abscess measuring 4.1 × 4.7 cm (Bezold abscess) without evidence of extension into the posterior fossa or dural venous sinus thrombosis as seen in Fig. 1. The CT also showed opacification of the middle ear cavity with slight erosive changes of the malleus, as seen in Fig. 2. The chest X-ray showed mild hyperexpansion of the lungs with no evidence of bacterial pneumonia, stable mild to moderate bilateral narrowing of the upper intrathoracic tracheal air shadow, normal heart size, and mild to moderate parahilar peribronchial cuffing indicative of viral infection or bronchitis.
In the ED, the patient was given two 500 mL boluses of intravenous fluids, one dose of 1250 mg of vancomycin, one dose of 2 g of cefepime, 3 mL of ipraptropium bromide/albuterol sulfate every 8 hours, and methylprednisone. The patient was admitted to the inpatient team for antibiotics and surgical intervention. ENT specialist planned for urgent surgical intervention with incision and drainage, complete cortical mastoidectomy and right myringotomy, and tympanostomy tube placement. The patient was admitted for further management of complicated acute right-sided otitis media and comorbidities.
The patient successfully underwent emergent surgery with ENT specialist. The findings included an extensive suppurative process of the mastoid extending from the middle ear to the neck and keratinizing epithelium within the middle ear to mastoid transition (likely cholesteatoma). Cultures were obtained from the mastoid contents, middle ear, and neck abscess.
The patient was initially extubated postprocedure; however, he rapidly developed respiratory distress and acute hypoxic, hypercapnic respiratory failure with resultant reintubation postoperatively. Imaging with both chest X-ray and computed tomography angiography (CTA) chest revealed right bronchiolitis but otherwise unremarkable, and an endotracheal aspirate was sent for culture. Additionally, the patient was noted to have new-onset paroxysmal atrial fibrillation, which initially required amiodarone. However, after conversion to normal sinus rhythm and given the severity of his COPD, the care team elected for rate control with metoprolol tartrate.
The patient’s hospital course was initially complicated by recurrent fevers despite being on vancomycin and cefepime. Therefore, given the concern for inadequate anaerobe coverage, metronidazole was added to the regimen. Additionally, given the concern for extension of the infection to the epidural space and potential inadequate source control, the patient underwent magnetic resonance imaging (MRI) of the cervical spine and repeat CT maxillofacial, which were both nonrevealing beyond postoperative changes.
At 3 days postoperatively, the patient was successfully extubated and had no further respiratory distress noted throughout his hospital stay, with continued oxygen improvement to his home oxygen of 3 L by hospital day five. Throughout treatment, the patient’s blood cultures and endotracheal aspirate remained negative. However, operative cultures from the abscess ultimately grew Fusobacterium nucleatum, Prevotella oris, and Parvimonas micra (formerly Peptostreptococcus), and following the infectious disease team’s recommendations, antibiotics were narrowed to ampicillin-sulbactam at 3 g every 6 hours with an intended 2-week intravenous course followed by 2 weeks of oral amoxicillin/clavulanate. Given the organism that grew and the patient’s poor dentition, which revealed tenderness to palpation, a follow-up dental evaluation was recommended. The patient was discharged on postoperative day eight to a skilled nursing facility to complete the antibiotic course, with outpatient follow-up pending.. The patient has been riding his bike, walking short distances, regaining his appetite, and is recovering well.






Add Comment