A 33-year-old healthy gentleman was injured while riding a scooter without wearing a helmet. He had poor consciousness (E1V1M5) upon triage and brain computed tomography showed diffuse brain swelling, subarachnoid hemorrhage, and subdural hemorrhage. One month after the trauma, he regained consciousness and started to notice poor vision in both eyes. Upon ophthalmic examination, the vision was only with light perception in both eyes, the intraocular pressure was within the normal range, and the light reflexes were normal with no relative afferent pupillary defect. The lenses were clear but severe vitreous opacity obscured the viewing of both fundi. B-scan ultrasonography showed diffuse vitreous opacity with posterior vitreous detachments and no retinal detachment in both eyes, therefore close observation was suggested.
Three months later, the vitreous opacity remained, and the follow-up ultrasonography showed a stationary condition. After discussing with the patient and family, a vitrectomy was scheduled but later postponed due to an episode of hospital-acquired pneumonia. During the treatment of pneumonia, the patient received systemic corticosteroids (fludrocortisone acetate, administered orally 0.2 mg per day for eight days to address salt-wasting syndrome). Five months after the trauma, a vitrectomy in the right eye was arranged (Video 1). During the operation, a grade IV vitreous opacity was noted, and a careful vitrectomy was conducted. After clearing up most of the vitreous opacity, a peculiar brownish mass lesion was found covering the posterior pole, and the optic disc and macula could not be identified (Fig. 1A and B). Presumed to be an organized vitreous hemorrhage, the brownish mass was carefully removed by microforceps. During the process, severe adhesion of the mass lesion with the underlying retina was noted. After the successful removal of the mass, the optic disc could be seen, which was located directly under the mass.
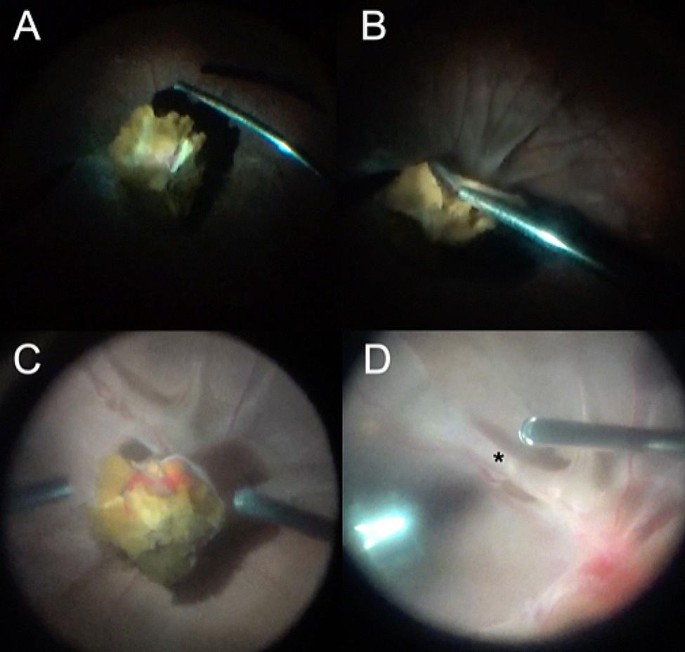
Intraoperative images of peculiar optic disc mass lesions and tractional retinal detachment in bilateral Terson syndrome. (A, B) A yellowish-pigmented lesion can be seen after core vitrectomy in the right eye. Severe retinal folds can be appreciated in (B). (C) During vitrectomy for the fellow eye, a similar lesion was found. (D) After removing the mass lesion, retinal folds were noted around the macula (asterisk)
Then, it was found that there was an extensive epiretinal membrane around the optic disc. These epiretinal membranes were thick, glutinous, multilayered, and very adherent to the underlying retinal tissue, therefore extremely difficult to remove (Video 1). An additional file explains Video 1 and Video 2 [see Additional file 1]. The perimacular traction related to the dense epiretinal membrane had caused a relatively flat tractional retinal detachment 360 degrees around the macula and formed a pouch-like configuration, which obscured direct viewing of the macula. After maximal efforts in peeling the epiretinal membrane, the macula could finally be visualized.
However, severe retinal folding around the macula persisted and could not be flattened even with the assistance of heavy liquids; therefore, laser coagulation was applied around the macula, and 5000 centistoke silicon oil was injected for long-term tamponade. Intraocular bleeding was controlled by diathermy.
Two days later, surgery was performed on the fellow eye (Video 2). Very similar findings were noted, with a dense vitreous opacity, peculiar brownish mass-lesion on the optic disc, and multilayered epiretinal membrane around the optic disc and covering the macula (Fig. 1). Fortunately, the macula could still be seen and there was no pouch-like tractional retinal detachment around the macula. Epiretinal membrane peeling was done to release the traction and 5000 centistoke silicon oil was used for tamponade after meticulous cauterization.
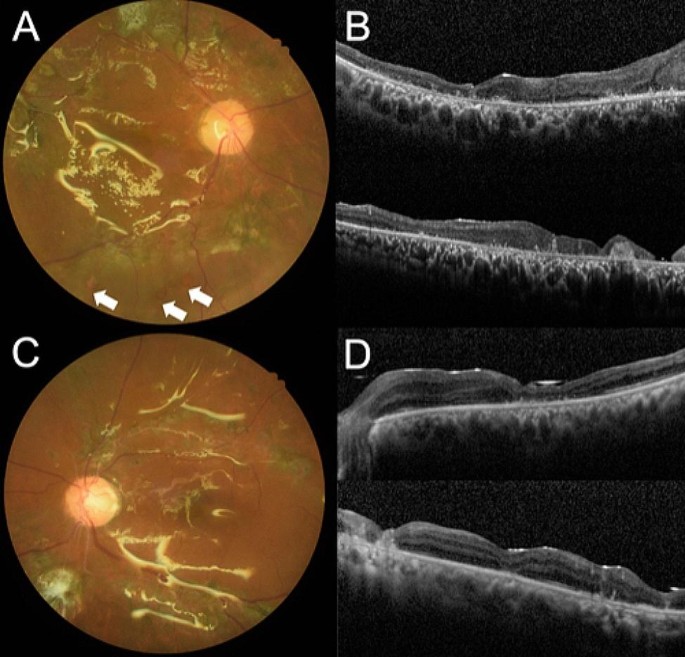
Eight months after the surgery, inferior redetachment was noted in the right eye despite silicon oil tamponade and vision remained poor at hand motion (Fig. 2A and B). In the left eye, the retina was well-attached after silicon oil and cataract extraction six months after the initial surgery (Fig. 2C and D). His vision in the left eye improved to 20/100.
Postoperative color fundus photographs and optical coherence tomography images. (A) Inferior retinal breaks (arrows) and redetachment were noted in the right eye despite silicon oil tamponade. (B) The macula was atrophic. (C) The retina was well-attached in the left eye after silicon oil removal and the macula was relatively preserved (D)




Add Comment