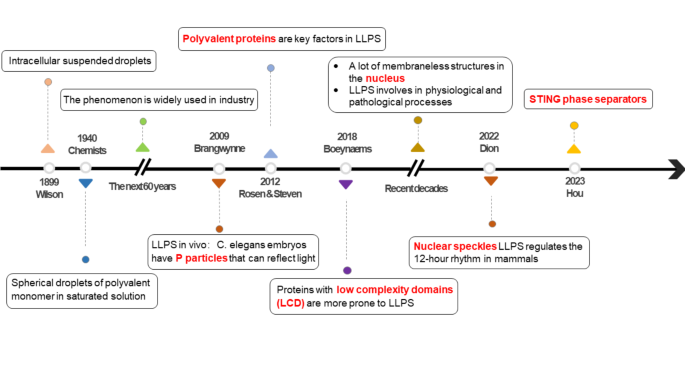
The research history of LLPS
Brangwynne was the first to discover the liquid reflecting light in C. elegans embryo, also known as, P particles, which exhibit liquid-like behavior, such as dissolution, condensation, and attachment, they indicate intermolecular interaction within the cytoplasm [14]. In 2012, cryo-electron microscopy demonstrated that proteins rich in repeated charged amino acid residues and with multiple folded domains (such as the SH3 domain) contribute to LLPS [15]. In recent years, it has been approved that proteins with low complexity domain (LCD) were easier to drive LLPS through weak interactions between their amino acid residues. For example, fused fused in sarcoma (FUS) relies on tyrosine or phenylalanine residues to achieve LLPS [16] (Fig. 1).
Biomolecular Condensates in eukaryotic cells. A) Schematic of the numerous condensates in the nucleus, cytoplasm, and membranes, such as stress granule, Cajal body, P-body, nuclear speckles, et al. B) Internal structure model of condensates. For example, the stress granule is driven by liquid-liquid phase separation. It is composed of proteins and RNA from the dispersed state into a highly aggregated droplet-like structure, which displays liquid-like properties
With the development of bioinformatics algorithms, more specific structures and functions of LLPS have been reported. Significantly, LLPS-regulated membraneless structures are abundant in mammalian cells [17, 18]. Nucleolus is an insoluble droplet composed of RNA and protein, which displays liquid-like viscous relaxation and effective surface tension [19]. As a self-protection mechanism for cell growth and survival, when eukaryotes face external stress, mRNA and protein are packaged into ribonucleoprotein particles, namely stress granules (SGs). When specific conditions are activated, translation can be restarted [20]. Intervention in the assembly and depolymerization of biomolecular aggregates such as SGs provide new ideas for the diagnosis of diseases (Fig. 2).
Formation conditions
Polyvalent molecules in biomolecular condensates naturally tend to aggregate into a large polymer in a heterogeneous state, similar to the layering and isolation of two phases in vinaigrettes, which reduce the solubility, thus contributing to LLPS [21]. LLPS is driven when the macromolecular components in high concentrations, exhibit a stronger affinity for each other compared to cytoplasmic molecules, and different phases are equal in chemical potentials [21, 22]. Eventually, surface tension leads to the spherical structure.
Importantly, it has been indicated that the LCD, intrinsically disordered region (IDR), and weak polyvalent interactions of the protein serve as triggers for LLPS [1]. Weak interactions, such as π-π interactions [23], cation-π interactions [24], electrostatic interactions [25], and transient cross-β contacts [26]. LLPS exhibits a remarkably dynamic and rapid ability to interact with the external environment in biomolecular condensates. Indeed, any perturbation that influences protein structures or intermolecular contacts can disturb LLPS behavior.
Exogenous infections can also evoke LLPS. Viral infection can lead to protein aggregation, which may be due to the exogenous nucleic acid molecules stimulating and attracting a substantial quantity of antiviral immune molecules. For instance, heat shock proteins are frequently integrated into virions via LLPS to facilitate the assembly and enhance the proteins’ stability [27].
Regulation methods
Physicochemical property and post-translational modification (PTM) regulate LLPS
The alteration of physical and chemical properties is the fundamental element for LLPS, such as component concentration, temperature, pH, valency, salt concentration, and PTM of proteins, like phosphorylation, methylation, ubiquitination, acetylation, etc. [28, 29]. Proteomic analysis has successfully identified a total of 14 serine or threonine phosphorylation sites on LCR [26, 30]. Sang has shown that the C-terminal fragment of MAPK3 will accelerate the serine site phosphorylation of substrate ELK1 after recruitment. This finding suggests that the condensate itself can modulate the new links in the LLPS network by increasing the phosphorylation rate [31]. Furthermore, the methylation of arginine residues can enhance the hydrophobic properties of RNA-binding proteins, like FUS, consequently impeding LLPS.
PTMs are closely associated with a variety of diseases, including cardiovascular disorders, liver diseases, and neurological disorders [32]. They play a crucial role in coordinating gene expression, metabolic reprogramming, and immune recognition. Deviations in these modification levels can lead to genomic abnormalities, cellular metabolic disruptions, and immune evasion [33]. Consequently, PTMs influence LLPS by changing the charge distribution and hydrophobicity of key protein IDRs, which encompasses both up-regulation and down-regulation, further impacting disease progression.
Certain core molecules regulate LLPS
LLPS is regulated by several “switch” molecules including GAP SH3 Binding Protein 1 (G3BP1), G3BP2, ATP, etc. Cells can produce SGs to protect themselves from damage under stress [34]. As a structural composition of SGs, G3BP1 possesses a nuclear transport 2-like domain, an inherently disordered region, and an RNA binding domain that contains RNA-recognized and RGG motifs. Under no-stress conditions, G3BP1 is in a closed conformation [35]. Under external stimulation, an elevated RNA in the cell induces RNA-dependent LLPS, causing a change into an open G3BP1 conformation. During this, the RGG domain binds to RNA, and phosphorylation occurs at S149, which promotes LLPS [36]. Further studies have revealed that the interaction between Caprin1 and G3BP1 with NTF2 can enhance the formation of SGs. Conversely, USP10 acts as a negative regulator of SGs assembly by obstructing the binding site of NTF2 [37]. In addition, it has been confirmed that ATP can also promote LLPS, for example, free nucleotides promote the formation of droplets in nucleosomes within H1 chromatin. This finding highlights the potential role of energy molecules in LLPS regulation [38]. Recently, 1,518 endogenous phase-separating proteins have yet to be discovered in a quantitative and high-throughput manner [39]. Therefore, we look forward to more factors involved in LLPS assembly to develop precise molecular targets.
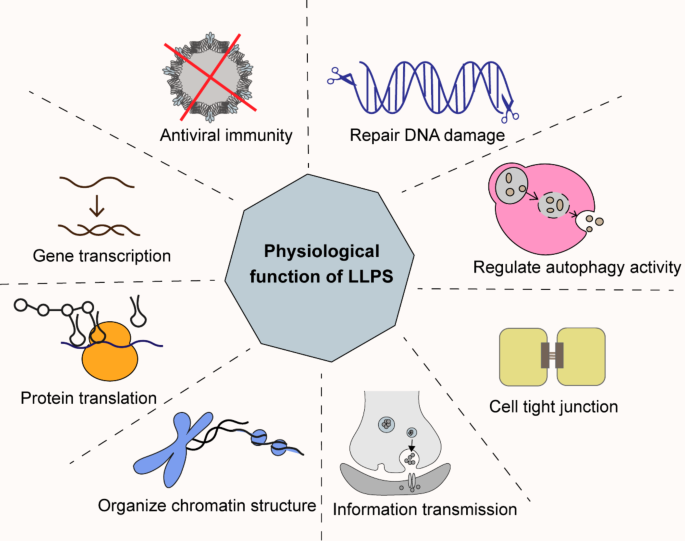
The physiological function of LLPS
Gene transcription and protein translation
The core proteins involved in transcriptional activation are formed through LLPS aggregation, including RNA polymerase II, transcription factors, coactivators, and elongation factors [40]. During transcription initiation, LLPS recruits Pol II to gather at active gene sites and enhances concentration between DNA and transcription factors to form the transcription initiation complex [41]. During transcription elongation, the C-terminal domain of Pol II is phosphorylated by the transcription elongation factor P-TEFb, and aggregates with other proteins, ultimately leading to complete the transcription [30]. Interestingly, super-enhancers are formed by transcription factors and co-activators through LLPS, which may provide insights into the excessive activation of tumor genes [42] (Fig. 3).
Translating RNA into proteins also requires LLPS. Recent studies have provided evidence that ATXN2 facilitates the translation of the circadian rhythm protein PER2 through binding within its AUUUU/A motif in RNA [43]. This finding opens a novel perspective for future investigations into the trans-spatial and temporal regulation of diverse cellular activities via LLPS [44] SGs is conducive to cell survival [45]. In virus-induced stress response, the cell’s protein translation is inhibited. At the same time, eukaryotic initiation factor 2α kinase in SGs can efficiently activate NF-κB and IRF3 on the innate immune signaling pathway, which recruits antiviral proteins and initiates antiviral response [46].
Chromatin organization
Chromatin is a condensed and organized structure composed of histones and DNA. LLPS plays a crucial role in chromatin compartmentalization [47]. Protein purification experiments initially revealed that heterochromatin protein 1 (HP1) possesses the capability to create LLPS droplets, and it will be considerably diminished when lysine is substituted with an uncharged amino acid [48]. Furthermore, HP1 is more prone to form droplets when interacting with single-stranded DNA compared to double-stranded DNA [49]. Another study found that methyl-CPG binding protein 2 can induce LLPS in vitro and compete with histone HP1 to generate chromatin condensates. Besides, the binding of methyl-CPG protein 2 to DNA makes it easier to form chromatin condensates [50, 51].
Signal transduction
Various signaling pathways rely on LLPS, such as RTK, Hippo, JAK-STAT3, and mTOR signaling pathways. The RTK signaling pathway depends on the phosphorylation of a terpolymer complex, which contains fibroblast growth factor receptor 2, the phosphatase SHP2 and PLCγ1. It serves as a scaffold to interact with downstream molecules on the plasma membrane [52, 53]. In the Hippo signaling pathway, the core protein kinase LATS2 forms a condensate and recruits important components to promote signaling activation and the cells’ apoptosis [54].
LLPS exists in the synaptic transmission. The postsynaptic density is a membraneless structure located beneath the postsynaptic plasma membrane and is characterized by proteins in high concentrations, where the cognitively deficient synaptic-associated protein SynGAP interacts with PSD-95 via LLPS [55, 56]. In conclusion, the optimal level of LLPS is necessary for transmission within cellular systems.
LLPS in liver innate immune signaling pathways
cGAS-STING pathway
The cGAS-STING pathway is robust in DNA sensing and innate immune response [57]. Following viral infection and cellular damage, there is a notable increase in DNA concentration within the cytoplasm. Subsequently, a cGAS-dsDNA complex is created into a high-concentration droplet via LLPS, which induces the catalytic domain rearrangement of cGAS, ultimately leading to the synthesis of cyclic GMP-AMP (cAMP). In the resting state, STING is primarily localized in the ER [58]. Upon binding of the cyclic GMP-AMP (cGAMP), it performs a conformational change and transfers to the Golgi apparatus. In fact, the translocation event is accompanied by post-translational modifications and subsequent activation of TBK1. Then, IRF3 recruited by STING will be phosphorylated by TBK1, then translocating into the nucleus as a dimer to regulate the transcription of type I IFN [59, 60]. (Fig. 4) At present, nanoparticle-delivered Svg3 has shown great potential as a cGAS agonist oligonucleotide in cancer combination immunotherapy [61].
Schematic model of cGAS-STING and RIG-I-MAVS signaling pathway via LLPS. After sensing and recognizing DNA from itself or viruses, cGAS will combine with DNA and assemble into a complex. The cGAS-DNA droplets activate cGAMP, which further binds to STING on the endoplasmic reticulum membrane and activates the STING-TBK1-IRF3 axis, eventually inducing type I IFN expression. After DNA viral infection, RIG-I will detect RNA quickly. When binding to the K63 polyubiquitin chain, RIG-I interacts with MAVS through their CARD domain. Subsequently, a fraction of MAVS molecules will undergo initial aggregation via LLPS, and then more MAVS molecules form a large condensate, which triggers the RIG-I signal cascade and causes the activation of NF-κB, resulting in the type I IFN expression. Too high concentration of cGAMP can induce STING to pull ER together and form a cubic membrane-like structure, which hinders downstream signal transduction [62]. Obviously, cells regulate the cGAS-STING pathway through LLPS to maintain the optimal level of innate immunity, which enables cells to effectively counteract external pathogens while safeguarding their own tissues from harm. ATP: adenosine triphosphate; GTP: guanosine triphosphate; cGAS: cyclic GMP-AMP synthase; cGAMP: cyclic GMP-AMP; STING: stimulator of interferon genes; TBK1: TANK-binding kinase 1; IKK: inhibitor of kappa B kinase; IRF3: interferon regulatory factor 3; NF-kB: nuclear factor kappa-B; RIG-I: retinoic acid-inducible gene I protein; MAVS: mitochondrial antiviral signaling protein; CARD: caspase activation and recruitment domains
RIG-I-MAVS pathway
RIG-I is an RNA sensor in the innate immune response. It is expressed not only in immune cells but also in hepatocytes [63]. As an adapter protein in the downstream signal transduction, MAVS interacts with RIG-I by their caspase activation and recruitment domains (CARDs). Additionally, MAVS possesses a short transmembrane domain at its C-terminal region responsible for anchoring itself to the mitochondria membrane [64]. In virus-infected cells, RIG-I detects viral RNA, and upon binding to the K63 polyubiquitin chain, RIG-I combines with MAVS. A fraction of MAVS molecules undergoes initial aggregation via LLPS, followed by subsequent recruitment of more MAVS molecules to form larger condensates. It triggers the RIG-I signal cascade and leads to the activation of NF-κB and IRF3, resulting in the type I IFN gene expression [65]. Therefore, the balance of RIG-I-MAVS is crucial in liver diseases, especially those caused by concomitant viral infections.
Inflammasome pathway
Inflammasome is a polymeric protein complex that triggers inflammation in response to exogenous pathogens or endogenous danger signals. This complex is composed of a sensor (a member of the NLR family), an adaptor protein (apoptosis-associated speck-like protein), and an effector protein (procaspase-1) [66]. In liver disease, the NLR family involved in inflammasome includes NLRP1, NLRP3, NLRP6, NLRC4, and AIM2 [67]. In the canonical inflammasome pathway, the inflammasome promotes the secretion of IL-1β, IL-18, and IL-33, and causes a systemic or local inflammatory response to initiate pyroptosis [68].
Fluorescence recovery after photobleaching has found that dsRNA can induce NLRP6 with multiple repeated lysines to emerge LLPS in vitro. NLRP6-dsRNA droplets are highly dynamic, and a hepatitis virus-infected mice model further confirmed the NLRP6 condensates in vivo [69]. It explains that LLPS acts as a switch to start the inflammatory response so that it integrates various signals and resists the external virus attack in an orderly manner.
Autophagy
Autophagy is an ancient innate immune homeostatic process that clears cytoplasmic protein aggregates or engulfs extracellular debris through mitochondria and lysosomes [70]. Theoretically, autophagy possesses anti-inflammatory functions [71]. It can degrade liquid condensates, and the pre-autophagosomal structure also undergoes LLPS to regulate autophagosome [72]. Studies have shown that LLPS is involved in selective autophagy, where droplets containing p62 and receptor proteins determine the direction of the isolation membrane extension [73]. Droplet-like p62 can recognize polyubiquitin chains on target proteins, which then recruit autophagy-related proteins such as ATG8 to form autophagosomes, thereby promoting autophagic degradation [74]. Clinically, this mechanism has been confirmed to provide protective effects against Huntington protein-induced cell death [75]. p62 is a common component of many disease-associated cellular inclusions, such as Mallory-Denk bodies, which are present in alcoholic hepatitis and alcoholic cirrhosis patients. Therefore, specifically targeting and degrading pathogenic proteins in the liver by controlling linker protein LLPS appears to be a promising and innovative therapeutic strategy.
Research indicates that dysregulation of autophagy is associated with various liver diseases [76]. Intracellular proteins can condense into LLPS droplets under certain physicochemical conditions. These cytotoxic protein aggregates are selectively degraded via autophagy. For instance, autophagy intersects with lipid homeostasis, where lipid droplets may mediate the breakdown through LLPS, thereby providing energy for the liver [77].
Liver innate immunity and diseases
Emerging evidence extends that overactivated innate immunity may contribute to liver disorders, including viral hepatitis, non-viral hepatitis, non-alcoholic fatty liver disease (NAFLD), liver fibrosis, liver ischemia-reperfusion injury (IRI), autoimmune liver disease (ALD), and liver cancer [78]. Therefore, we aim to artificially manipulate the strength of the liver’s innate immunity utilizing the regulatory law of LLPS (Fig. 5) (Fig. 6) (Table 1).
A model of liver diseases with innate immune inflammation as the central link. The liver is an immune organ with abundant innate immune cells including kupffer cells and natural killer cells. Hepatic stellate cells and endothelial cells are also involved in liver innate immunity. This induces inflammation and promotes the production of many inflammatory cytokines, which contribute to various liver diseases as shown in the figure. IFN: Interferon; IRF3: interferon regulatory factor 3; TNF: tumor necrosis factor; ROS: reactive oxygen species
A pattern diagram of LLPS involvement in different liver constituent cells. The liver is an immune organ composed of various cells, including hepatocytes, Kupffer cells, epithelial cells, hepatic stellate cells, and immune cells (e.g. NK cells, T cells, and B cells). Hepatocytes contain abundant LLPS, including cccDNA, p62, NLRP6, glycogen molecules, and MAVS-STING. KCs contain lncRNA MALR-ILF3 and phagocytic protein WIP/WASP droplets. Different cells perform specific physiological functions to maintain homeostasis or impact disease progression driven by LLPS. cGAS: cyclic GMP-AMP synthase; LLPS: liquid-liquid phase separation; NK: natural killer; SG: stress granules; STING: stimulator of interferon genes; TNFα: tumor necrosis factor-α; DDX3X: DEAD-box helicase; cccDNA: covalently closed circular DNA; p62: Sequestosome 1; ATG8: autophagy-related proteins; Keap1: kelch like ECH associated protein 1; Nrf2: nuclear factor-erythroid 2-related factor 2; WASP: Wiskott–Aldrich syndrome protein; WIP: WASP-interacting protein; MALR: mammalian apparent long terminal repeat (LTR) retrotransposons; ILF3: interleukin enhancer binding factor 3; HIF1α: hypoxia-inducible factor 1α; NLRP3: NOD-like receptor family pyrin domain containing 3
Viral hepatitis
Viral hepatitis is an infectious disease caused by multiple hepatitis viruses, the most common being hepatitis B virus (HBV) and hepatitis C virus (HCV). The strength of the antiviral immune response depends on the LLPS in the immune pathway [79, 80]. The cGAS-STING pathway and hepatitis virus infection are interdependent. On the one hand, by recognizing nucleic acid components, cGAS-STING prevents viral replication by initiating downstream inflammatory factors [81]. On the other hand, hepatitis viruses evade the cGAS sensing by employing many tactics. For example, the hepatitis B virus X protein (HBx) directly stimulates the ubiquitination and autophagic degradation of cGAS, which down-regulates the production of type I IFN [82]. HCV disrupts the interaction between STING and TBK1 by NS4B proteases to inhibit RNA-induced IFN activation [83].
RIG-I targeting activation has been confirmed as a new treatment for viral hepatitis. The long-term existence of cccDNA in the hepatocyte nucleus is typical for chronic HBV hepatitis [84]. RIG-I agonists can effectively resist cccDNA by activating immune responses [85]. In a study, the co-delivery of siRNA targeting HBx and IL-12 plasmid to hepatocytes upregulates MAVS and RIG-I, thereby reversing virus-induced immune suppression [86]. Interestingly, cccDNA undergoes LLPS in a G-quadruplex-dependent manner, which accelerates HBV propagation within liver cells. This suggests that disrupting the stability of G4 structures may offer a potential strategy to alleviate chronic infections [87]. In HCV-infected hepatocytes, the expression of RIG-I and MDA5 is significantly decreased compared with other PRRs, which reveals that signal amplification of RIG-I-MAVS may serve as a crucial target for antiviral immunotherapy [88]. It is worth noting that HCV uses innate pathways to exploit its infectious advantage, thereby promoting HCV self-assembly and hepatic lipogenesis [89].
Both HBV and HCV infections impair autophagic flux [90, 91]. The HBx and HCV NS5B enhance the autophagosome formation in liver cells [92]. HBx reduces lysosomal targeting by interacting with V-ATPase, thereby impairing autophagic degradation. On the other hand, HCV defects autophagic flux by disrupting the fusion of autophagosomes with lysosomes [93]. Therefore, autophagy can serve both as an antiviral defense mechanism and as a process that supports viral replication.
Non-viral hepatitis
Non-viral hepatitis refers to a group of hepatitis mainly including steatohepatitis, alcoholic hepatitis, and drug-induced liver injury (DILI) [94]. Continuous and prolonged hepatic cellular oxidative stress and liver inflammatory stimuli are key signatures of DILI. Excessive acetaminophen can promote the production of reactive oxygen species (ROS) and induce mitochondria to release mtDNA, thus activating the cGAS-STING [104]. Hepatocyte DDX3X protects against DILI by controlling SGs formation and oxidative stress [95]. Acetylation of the IDR region in DDX3X is essential for enhancing LLPS propensity and SG maturation. The deacetylase SIRT6 is a critical regulator of SGs [105]. Therefore, specific acetylation modifications are closely associated with liver diseases.
Autophagy can protect against DILI by selectively removing damaged mitochondria and drug conjugates. For example, chlorpromazine alleviates DILI by activating autophagy [106]. Additionally, IL-22 prevents DILI in mice by activating AMPK-dependent autophagy [107]. Therefore, targeted autophagy presents an effective strategy for the prevention of DILI.
NAFLD
NAFLD is the most common chronic liver disease worldwide [108]. For example, a high-fat diet can activate the cGAS-STING response in adipose tissue, further leading to obesity, insulin resistance, and metabolic dysfunction [109]. Immunohistochemistry has shown that STING levels in hepatocytes of NAFLD are higher than those of non-NAFLD. On the contrary, loss of STING in macrophages mitigates hepatic steatosis and reduces serum levels of cholesterol, triglycerides, and low-density lipoproteins [110, 111]. In addition, lipid overload in hepatocytes leads to replication stress and DNA damage, which stimulates specific upregulation of cGAS-STING [112]. These suggest that the inflammatory response and the lipid metabolism disorder are mutually reinforcing.
The dysregulated immunity contributes to the transformation of non-alcoholic fatty liver (NAFL) to non-alcoholic steatohepatitis (NASH) [113]. Immunohistochemical analysis of the human liver has shown that the RIG-I level of advanced NASH is significantly stronger than that of NAFL, besides, the mean IRF3 staining intensity in NASH bile duct is higher than that in NAFL [114]. The RIG-I-MAVS pathway plays a contributing role in the deterioration of NAFLD.
Autophagy serves as a protective mechanism against lipid toxicity in NAFLD. However, hepatic autophagy and lysosomal function are compromised in disease states, leading to more severe pathogenic steatosis [115, 116]. In hepatocytes, p62 and ATG8 form autophagosomes, and subsequently, Keap1 can bind within the p62 gel reversibly, activating the transcription factor Nrf2 [116] These findings suggest that p62 gels may function as a platform for Nrf2-mediated inflammatory responses. Further research is needed to elucidate the role of LLPS-mediated selective autophagy in liver diseases. Additionally, it is worth exploring whether enhancing liver lipid droplet clearance through the ubiquitin-proteasome system via LLPS could be a viable strategy.
PTMs are involved in NAFLD. A study indicates that acetyl-CoA helps limit the autophagic degradation of lipid droplets, acting as a key regulator of hepatic lipid homeostasis [117]. Evidence shows that deacetylase SIRT3 is reduced in NAFLD [118]. Additionally, the phosphorylated insulin-induced gene weakens its interaction with the E3 ubiquitin ligase gp78, thereby inhibiting hepatic lipogenesis [119]. Therefore, inhibiting acetyl-CoA production or modulating specific acetylation/ubiquitination in the liver could be a novel therapeutic option for NAFLD.
Liver fibrosis
In the process of chronic liver disease, excessive deposition and abnormal distribution within the extracellular matrix in the liver will lead to fibrosis. The activated KCs and hepatic stellate cells (HSCs) are the core pathogenesis of hepatic fibrosis [120, 98]. For example, X-box binding protein 1 can promote the mtDNA leakage from KCs and induce innate immunity [121]. Iron death in hepatocytes will cause oxidative DNA damage and stimulate STING in KCs, which establishes an activated immune microenvironment to promote liver injury and fibrosis [99]. Accordingly, the upregulation of cGAS-STING has been reported to aggravate liver inflammation in liver fibrosis patients and mice models [101]. However, activated cGAS-STING can inhibit endothelial cell proliferation, thus showing the potential to alleviate liver fibrosis [102]. To sum up, there is still controversy regarding the aggravating or mitigating effects of the cGAS-STING pathway on liver damage, and whether these effects are dominant in specific situations subject to further consideration.
Autophagy promotes HSC activation. In vitro studies have shown that autophagic activity significantly increases in fibrous mouse or human HSCs [122]. Various signaling pathways can activate autophagy in HSCs to promote fibrosis, such as the Akt/mTOR, ERK, and JNK pathways [116]. Additionally, p62 can directly bind to the vitamin D receptor and retinoid X receptor, urging their heterodimerization and thereby suppressing HSC activation [123]. Therefore, the accumulation of p62 due to autophagy inhibition may inhibit liver fibrosis through LLPS.
Liu ZY demonstrated that phosphorylation of heat shock protein 27 under stress enhances FUS LLPS, maintaining a liquid phase to prevent amyloid fibril formation [124]. Although no specific molecules have been identified that undergo spontaneous LLPS in liver fibrosis, it is possible that PTMs crosstalk-induced protein aggregation changes may occur in the context of complex stress disorders and extensive protein deposition.
IRI
IRI, manifested by innate immune-mediated inflammation and stress-induced oxidative damage, usually occurs after hepatectomy and liver transplantation, leading to liver dysfunction and transplant failure [125]. Hepatocytes release significant mtDNA during IRI, it will be recognized by cGAS-STING and contribute to the production of inflammatory cytokines, thus aggravating IRI [126]. Notably, cGAS-mediated autophagy can protect the liver in a STING-independent manner [127]. So, the localization pattern of STING in different cells, and the tissue specificity of cGAS-STING pathway both remain to be explored.
Previous studies have found that ROS secreted by IRI contributes to the MAVS activation and further LLPS aggregation in vivo, which finally excites downstream inflammatory pathways [128]. Paradoxically, new experiments demonstrated that reduced MAVS expression can enhance apoptosis and mitophagy in IRI, accompanied by higher plasma alanine aminotransferase and tumor necrosis factor-α [129]. It indicates a protective role for MAVS in liver inflammation.
ALD
ALD is a special chronic liver disease caused by immune dysfunction, including autoimmune hepatitis (AIH), primary biliary cholangitis, and primary sclerosing cholangitis (PSC). Droplets formed by cGAS and DNA inhibit the nuclease TREX1, this limits self-DNA degradation and leads to immune overactivation, finally resulting in AIH [130] In the AIH mice model, overload manganese establishes a hepatic inflammatory microenvironment and aggravates liver injury by activating the cGAS-STING pathway [131]. Drugs targeting the LLPS of cGAS-DNA may offer a valid treatment for AIH and other autoimmune diseases. However, the cGAS-STING pathway in other ALDs is rarely reported.
The dual role of NLRP3 inflammasomes in PSC has been confirmed. On the one hand, by releasing inflammatory factors to increase liver injury and fibrosis. For example, studies have shown that galectin 3 can activate NLRP3 inflammasome in KCs and HSCs to drive primary biliary cholangitis [103]. On the other hand, blocking other cell death pathways protects the PSC during acute cholestasis liver damage [132]. It can be seen that the innate immune and the cell death pathways interact to affect the balance of liver disease states.
Liver cancer
Liver cancer is a primary malignant tumor derived by persistent chronic liver damage, inflammation, and compensatory hyperplasia [133]. cGAS-STING recruits immune cells to gather and clear cancer cells by enhancing their susceptibility to immune attack by NK cells and CTLs [134]. Currently, STING agonists are used as adjuvants in cancer vaccines by activating anti-tumor immunity [12]. Interestingly, the activation of the intrinsic cGAS-STING pathway in cancer cells also mediates immune cloaking after radiation therapy-induced DNA damage [135].
We consider RIG-I as a tumor suppressor, and overloaded RIG-I expression will be against proliferation, migration, and invasion of cancer cells [136]. A study found that in the diethylnitrosamine-induced HCC development model, the demethylase JMJD4 can demethylate RIG-I and prevent the IL-6-STAT3 signaling pathway to impair anti-tumor immunity. In other words, reduced RIG-I in carcinoma progenitor cells drives progression from HcPC to HCC [137]. It should be pointed out that RIG-I binds with STAT to amplify the IFN reaction in the above study [63]. Therefore, whether RIG-I has crosstalk and additional effects between the two pathways in viral HCC still needs to be verified.
Autophagy inhibits tumors, and defects in autophagy can promote liver cancer. The activation of oncogenes or loss of tumor suppressor genes can lead to mTORC1 activation [138]. Dysregulation of the p62-Keap1-Nrf2 axis has been observed in human and mouse HCC. The increased Keap1-p62 aggregates are associated with improved liver function [96]. Therefore, accelerating early autophagosome formation and autophagic protein aggregation through LLPS could be a potential therapeutic approach to liver cancer.
PTMs play a crucial role in cancer progression. N6-methyladenosine exerts biological effects by dynamically regulating methylation levels, including immunity, tumorigenesis, and adipogenesis [139]. The coiled-coil (CC) domain of the ubiquitin ligase RNF214 promotes the growth and migration of HCC through LLPS [140]. Additionally, SIRT1 is overexpressed in HCC, it promotes HCC in an obesity-dependent manner and involves crosstalk with mRNA methylation, protein acetylation, and ubiquitination [141]. Thus, PTMs of proteins or RNA influence their biomolecular aggregation through LLPS and may serve as biomarkers for early diagnosis of liver cancer.
Biomolecular condensates in liver cancer
LLPS enhances oncogenic signaling pathways and advances cancer progression, and has been proposed as a promising cancer biomarker and intervention target. In addition to the above-mentioned pathways, biomolecular condensates formed by other molecules are present in liver cancer [100].
Crafty tumors take advantage of LLPS as a strategy to evade innate immunity. For example, the cells’ growth needs more glucose consumption, when LLPS occurs in sufficient glycogen, the Laforin-Mst1/2 complex is wrapped together, which jointly activates the oncoprotein Yap, leading to liver growth and tumor transformation [97]. Recent evidence revealed that the acetyltransferase KAT8 and IRF1 will form a droplet and localize to the PD-L1 promoter, prompting the transcription and expression of PD-L1 [142]. In addition, the fusion oncoprotein PKA, which is linked to atypical liver cancer, can effectively block cAMP LLPS and result in abnormal signaling [143]. There are many other mutant proteins that improve the survival advantage and chemotherapy resistance of tumor cells by disrupting LLPS, such as tumor suppressor factors SPOP, [144]. PTEN, [145]. USP42 [146], . and SHP2 [15].
LLPS has also been observed to exert an anti-tumor effect. RNA interference technology demonstrated that circVAMP3 acts as a molecular scaffold by facilitating the LLPS assembly of SGs with CAPRIN1. This subsequently suppresses cancerous proliferation and migration [147].
Anti-tumor therapy focused on LLPS
Abnormal LLPS are regarded as carcinogenic factors. At present, studies have confirmed that LLPS is involved in a variety of cancers by condensing oncoproteins and changing chromatin structure, such as liver cancer, lung cancer, kidney cancer, ovarian cancer, leukemia, etc. [148]. Therefore, this section discusses anti-tumor efforts focused on the whole cancers, not limited to HCC [149]. The application of single-molecule magnetic resonance, atomic force microscopy, and freezing electron microscopy, along with the LLPS protein database PhaSepDB have provided us with great convenience to deepen the understanding of LLPS [150, 151].
The fusion protein is a prevalent mechanism that LLPS contributes to cancer progression. Scientists developed a high-throughput screening technique known as DropScan to find compounds that can regulate abnormal LLPS condensates. It offers a wide possibility for cancer treatment by targeting condensate fusion protein [152]. Recently, a series of chemical probes have been developed that exhibit binding affinity sensitive to the LLPS microstructure, enabling visualization, quantitative analysis, and even manipulation [153].
Certain antitumor medications also can engage in agglomerate assembly. Wang et al. have revealed that adriamycin exhibits specific binding to histone HP1. It induces an overall conformational change via LLPS, which suggests the latent role of LLPS in boosting drug enrichment at specific sites [154].







Add Comment