Patient characteristics
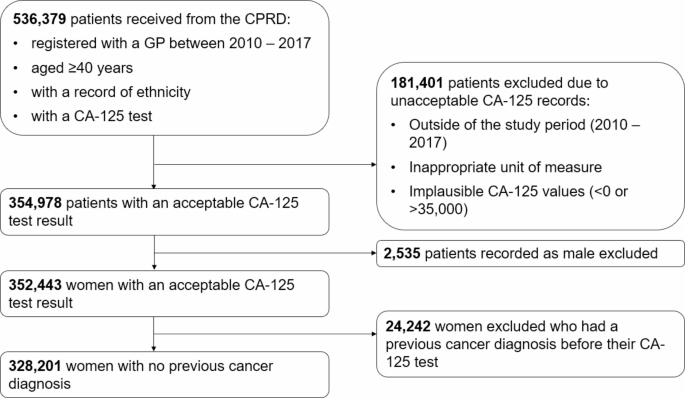
The cohort included 328,201 women aged ≥ 40 years with an acceptable CA-125 result in our study period with no prior cancer diagnosis (Fig. 1).
Patient characteristics are summarised in Table 1. A total of 328,201 women had a CA-125 test result in our study period (2010–2017). The majority were White (90%), followed by Asian (5%), and Black (3%). Women from the Other and Mixed ethnic groups each represented less than 1% of the study population, and there were 2,434 (< 1%) patients with record of unknown ethnicity who were included in the total figures. There were variations in patient characteristics across the ethnic groups. Most notably, White women were older (median 56 years vs. 50 years for both Asian and Black women) and Black women had higher deprivation scores (42% in the highest IMD quintile vs. 13% and 24% for White and Asian women, respectively). Median CA-125 levels were similar across the ethnic groups, although a lower proportion of White women had a high CA-125 result compared to Black and Asian women.
Ovarian cancer incidence
The one-year ovarian cancer incidence was 0.8% with 2,756 women in our cohort receiving an ovarian cancer diagnosis within one-year of their CA-125 test, including 2,589 White, 81 Asian, 43 Black, 10 Other, 10 Mixed, and 23 women with unknown ethnicity. There were too few ovarian cancer cases from the Mixed and Other groups to draw meaningful comparisons regarding ovarian cancer incidence. Consequently, these women were dropped from the analysis.
Table 2 outlines the one-year incidence of an ovarian cancer diagnosis and the incidence of an advanced stage diagnosis for White, Asian, and black women. White women were almost twice as likely to be diagnosed with ovarian cancer compared to Asian and black women (0.9% vs. 0.5% for both Asian and black women). Most women with ovarian cancer had an invasive epithelial ovarian cancer (≥ 95%) (supplementary 3). More black women were diagnosed with serous ovarian cancer than White or Asian women, and there were no black women in our cohort who were diagnosed with mucinous ovarian cancer (supplementary 3). Data on stage at diagnosis were available for 84% of patients. Black women were more likely to be diagnosed at an advanced stage compared to White and Asian women (67% vs. 58% for both White and Asian women). Median CA-125 levels in women with ovarian cancer were similar across the ethnic groups, however in women with advanced stage cancer they were higher for Asian women (751U/ml (95% CI 548 to 1,531U/ml)) compared to white women (496 U/ml (95% CI 462 to 531U/ml))
Diagnostic performance of CA-125 for predicting ovarian cancer, by ethnicity
The diagnostic performance of CA-125 is outlined in Table 3 for White, Asian, and Black women and the results for Other and Mixed women is supplied in Supplementary 4. A high CA-125 result had the highest sensitivity in the detection of ovarian cancer for Black women: 90.7% (95% CI 90.1 to 91.2%) vs. 79.4% (95% CI 79.3 to 79.6%) for White women and 71.6% (95% CI 70.9 to 72.3%) for Asian women. The specificity was marginally higher for White women: 93.8% (95% CI 93.7 to 93.9%) vs. 92.9% (95% CI 92.5 to 93.3%) for Asian women and 93.1% (95% CI 92.5 to 93.6%) for Black women. The positive predictive values (PPVs) of a high CA-125 result were approximately twice as high for White women: 10.2% (95% CI 10.1 to 10.3%) compared 4.9% (95% CI 4.6 to 5.3%) for Asian and 5.6% (95% CI 5.2 to 6.1%) for Black women. The negative predictive values were similar across the ethnic groups. The AUC was extremely high for all ethnic groups (≥ 0.90), but highest for Black women (0.96, 95% CI 0.92 to 0.99).
The diagnostic performance was largely unaffected following the exclusion of borderline tumours and women aged 50 years (Supplementary 4). In contrast to the unadjusted differences in PPVs of a high CA-125 result by ethnicity, adjustments for age group in 10-year categories, CMS, IMD, and year of test estimated the PPVs to be similar across all ethnic groups: 9.31% (95% CI 8.83 to 9.82) for White women, 7.84 (95% CI 6.06 to 10.1) for Asian women, and 8.39 (95% CI 6.12 to 11.4) for Black women. This reduction in differences was largely due to the adjustment for age-group (Supplementary 5).
The degree of association of an abnormal CA-125 result with incident ovarian cancer, relative to a normal result, differed significantly by ethnicity (interaction p-value = 0.02). However, adjustment for all covariates (age group in 10-year categories, CMS, IMD, and year of test), and for age group alone, nullified the interaction. The diagnostic odds ratio was over three times higher for Black women compared to White or Asian women: 187.4 (95% CI 66.4 to 528.4) for Black women, 70.7 (95% CI 64.0 to 78.2) for White women, and 55.8 (95% CI 33.8 to 92.2) for Asian women, although the confidence intervals for Black women were extremely wide so this was not a significant difference (Table 3).
The adjusted incidences and odds ratios of an incident ovarian cancer diagnosis for all ethnic groups can be found in Supplementary 6a. The results were largely unaffected when invasive ovarian cancer formed the outcome (Supplementary 6b).
Association of a high CA-125 result with the diagnosis of advanced stage ovarian cancer by ethnicity
For women who received an ovarian cancer diagnosis, the adjusted PPVs of an advanced stage diagnosis by CA-125 result were calculated. Adjustments were made for age group in 10-year categories, ovarian cancer histology, CMS, IMD, and year of test. The adjusted PPVs of an advanced stage diagnosis following a raised CA-125 result were similar for all women: 75.9% for White women (95% CI 72.6 to 78.9%), 69.6% for Asian women (95% CI 72.3 to 93.7), and 66.8% (95% CI 41.4 to 85.1) for Black women.
The point estimate of the odds ratio of being diagnosed at an advanced stage, relative to an early stage, following a raised CA-125 result in an ovarian cancer population was higher for Asian women (OR 15.7 (95% CI 2.66 to 93.1) vs. 6.08 (95% CI 4.13 to 8.96%) for White women and 0.40 (95% CI 0.02 to 9.25%) for Black women), although this was not significant. The degree of association between an elevated CA-125 result and being diagnosed with an advanced stage of ovarian cancer, relative to CA-125 result, did not differ by ethnicity.
A table of these results, including for the Other and Mixed ethnic groups can be found in Supplementary table 6c.
The estimated incidence of ovarian cancer by CA-125 level, by ethnicity
The predicted one-year incidence of ovarian cancer by CA-125 level and ethnicity for women aged ≥ 50 years is shown in Fig. 2. The overall estimated incidence of ovarian cancer at a CA-125 level of 35U/ml was 2.4% (95% CI 2.3 to 2.6%) and the estimated CA-125 level to correspond to a 3% incidence of ovarian cancer was 43 U/ml (95% CI 40 to 45 U/ml). These figures were similar for White women: 2.5% (95% CI 2.3 to 2.7%) and 41 U/ml (95% CI 39 to 44 U/ml), respectively. The predicted incidence for Asian women following a CA-125 level of 35U/ml was half the predicted incidence for White women (1.2%, 95% CI 0.8 to 1.8%). Similarly, Asian women reached the estimated 3% ovarian cancer incidence rate at higher CA-125 levels (69 U/ml (95% CI 52 to 89 U/ml)). For Black women, a CA-125 level of 35U/ml represented a lower estimated incidence of ovarian cancer (1.6%, 95% CI 0.9 to 2.8%) than White women, and a lower CA-125 level of 57 U/ml (95% CI 37 to 82 U/ml) to correspond to a predicted incidence rate of 3% of ovarian cancer. However, due to an insufficient number of Black women diagnosed with ovarian cancer aged ≥ 50 years, the confidence intervals were too wide to confirm differences.
The predicted incidence of ovarian cancer by CA-125 level and ethnicity for women aged ≥ 50 years up to 8%. The red line indicates the estimated CA-125 level to represent a 3% incidence of ovarian cancer and the dashed yellow line predicts the incidence of ovarian cancer at a CA-125 level of 35U/ml. The shading represents the 95% CIs.
Similar values were observed for the prediction of invasive ovarian cancers in women aged ≥ 50 years (Supplementary 7). The predicted incidence of ovarian cancer by CA-125 level and ethnicity for all women (including women aged ≥ 40 and the Other and Mixed ethnicities) can also be found in Supplementary 7.
Application of the ethnicity-specific thresholds resulted in increased specificity and PPVs for all ethnic groups, at the expense of sensitivity, particularly for Asian and Black women who would see a much larger reduction in sensitivity, and increase in false negatives, than White women. The diagnostic performance of the ethnicity-specific thresholds modelled in Fig. 2 is outlined in Supplementary 8a, along with a 2 × 2 table comparison of the ethnicity-specific thresholds and the current 35U/mL thresholds in Supplementary 8b.




Add Comment