Demographic characteristics of the patients
(Refer: Table 4– Demographic details of T2DM patients)
-
a.
Age: most of the interviewees belonged to the age group 35–60, with a mean age of 48 years.
-
b.
Education: The participant’s educational qualification ranges from SSLC to a bachelor’s degree. T2DM individuals with better educational qualifications bachelor’s degree n = 3/10.
-
c.
Gender: The study found that managing diabetes was particularly difficult for male participants who were the primary income earners for their families (80% of participants). This suggests a potential conflict between work demands and healthy self-management practices for male breadwinners.
-
d.
Occupation: The study showed that retired participants consistently followed DSM routines. This suggests that having a more flexible schedule might be beneficial for managing diabetes.
-
e.
Family income: The study discovered that among participants who belonged to the low-income group (earning less than 3 lakhs annually/ $3593.54/year), the cost was a significant barrier to effective DSM. One participant specifically mentioned rationing glucose strips due to their perceived expense.
-
f.
Duration of diabetes: The study suggests a link between consistent self-management and long-term glycemic control. Two participants with chronic diabetes who regularly monitored their blood sugar levels showed good adherence to self-management routines. Additionally, another participant diagnosed for over two years also demonstrated consistent self-management. All the participants recruited in this study belonged to rural areas of Karnataka state.
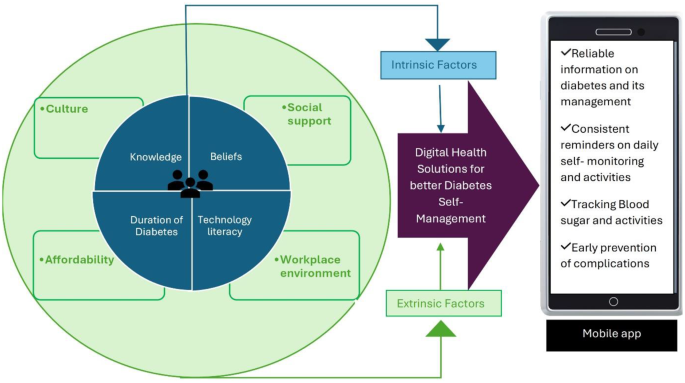
We have detailed perspectives of T2DM patients on the factors associated with self-managing diabetes, as well as understanding their needs using an ‘Empathy map’ given below in (Refer: Fig. 1).
Extrinsic factors influencing diabetes management among T2DM individuals: elaborating Fig. 1 below
[P – Indicates Patient responses]
Socioeconomic factors
-
a.
Culture: South Indian culture presents a unique challenge for T2DM patients due to the staple foods such as rice, rich in carbohydrates. Cultural preference for food among the south Indians clashes with traditional diabetic dietary advice given by their providers, making it difficult for individuals to manage their blood sugar through diet alone. Interviews revealed participant’s struggles in avoiding rice, highlighting the need for culturally sensitive approaches to T2DM management in South India.
P9- I feel I don’t have clarity on exactly the diet, I went to the dietician she has given me a chart to follow the diet. But still, I have carb items for my breakfast and diet.
To cater to the cultural needs, there is a need for culturally sensitive mHealth apps that provide healthy alternatives to traditional food ensuring low carbohydrate content, without compromising DSM.
-
b.
Social Support: The study identified social support as a crucial factor in T2DM management. Family members had a significant role in helping patients to navigate online resources, for example using a Google search engine to understand diabetes and find information on managing nutrition. While 50% (n = 5) appreciated support from doctors and HCPs, 40% (n = 4) highlighted the positive impact of family and peers. The family support system assisted with medication adherence, knowledge acquisition, and overall, self-management. However, despite strong support from physicians, family, and friends, challenges persisted in managing aspects like diet and exercise.
Quote on supportive family: P8- I don’t know how to use mobile phones; my children help me with it.
The study highlighted the importance of social support from family members in encouraging the use of phones, similar motivators from close family circles and HCPs could build trust and relieve anxiety among the individuals. By fostering motivation information sharing and accountability, social support can empower individuals to manage diabetes through mHealth apps,
-
c.
Workplace environment: Time constraints emerged as a significant barrier, particularly for the breadwinner of the family. Busy work schedules often faced by male participants, hindered effective diabetes management. Similarly, some female participants, primarily responsible for household chores have also reported challenges due to time limitations.
P7- I have no time left after my hectic work schedule.
P5- I find it difficult to manage because I go to work and in between, I can’t concentrate to check sugars and have medicines.
P7- No, also I don’t get enough time because of my job and hence I cannot do it.
These findings highlight the need for flexible DSM strategies that include using mHealth apps to access and initiate better management that can accommodate busy lifestyles.
-
d.
Affordability: The participants felt the cost of the glucometer and strips was high and as a result, they could not monitor blood glucose regularly.
Quote supporting the statement given by the study participants-
P2- I don’t check my sugar daily; I get my legs swollen, then I realize my sugar has spiked and do the sugar check. Or it’s too expensive to check every time the sugar levels.
P2- I monitor usually but sometimes I can’t correctly see, so I need to use a lot of time and spend money on extra strips and needles. So, I don’t check often.
Diabetes management requires various expenses including medication, blood glucose monitoring supplies, consultation fees, and quality food choices resulting in a significant financial burden on the patient or their family with limited income or inadequate health insurance facilities. The digital health solution here can be optimizing a mHealth app, with collective features including doctor appointments at a low cost, providing options for budget-friendly quality food choices, also having reliable educational content on testing blood glucose, unnecessary pricking of fingers to test, and unnecessary wasting of the strips, thus reducing the expenses incurred.
Intrinsic factors influencing DSM among T2DM individuals
Knowledge of effective DSM
Knowledge of DSM is associated with daily activities such as taking medication, diet, exercise, and blood glucose monitoring. Poor knowledge of managing diabetes was found among the T2DM individual’s reasons for this were that they were unaware of their condition at the initial phase of diagnosis and how they could manage it in their daily lives. A concern reported by the T2DM individuals on difficulties faced in managing diabetes is-.
Confusion to manage hypo and hyperglycemic levels
Fluctuations in the glycemic levels pre- and post-meal among the individuals confused medication adjustments.
P4- Sometimes the GRBS count comes up to 400 or 500 so then it’s a problem on what to do and how to control it. So, I take medications but when I take insulin then I get weak. My limbs shiver. So, then the doctor advised me not to continue insulin.
This suggests a difficulty in decision-making among the patients. The need for reliable education on what to do and being prepared is crucial in this situation. The Health app could provide an educational module on fluctuations in blood glucose and how to interpret them in the context, which can be beneficial. This can empower patients to better decision-making and avoid confusion.
Beliefs
One of the T2DM individuals exhibits distrust of conventional medicine. The patient was likely to be concerned over the potential side effects of medications and particularly believed that they would eventually get their kidneys damaged. They would rather try Ayurvedic treatment for their cure (a traditional Indian system of medicine known for its focus on natural remedies and holistic well-being).
P 2- I first began with the ayurvedic med and then I shifted to allopathic.
Educating patients on the limitations of other kinds of treatment from a healthcare provider is necessary and communicating this problem with a larger population addressing patient’s concerns and explaining benefits using digital platforms like mHealth apps or media could be effective in reaching the desired population in aiding them to make an informed decision.
Technology literacy
A. Poor technology literacy: Particularly elderly individuals who may not have grown up with modern technology or had limited exposure to it. The study revealed a digital divide among the older adults with T2DM. Limited technology literacy made it difficult for them to navigate search or utilize search engines effectively. This made them dependent on the younger generation, family, and friends to access the information and hindered their ability to access and manage diabetes independently and effectively. Eventually, as reported by some of the participants, after a dependent phase on family members to access diabetes-related information by navigating online and making their self-decisions on certain food choices.
P1- I don’t know how to use it; I must take my kids’ help for it. I check my GRBS daily so I must control my diabetes and I will ask my Daughter-in-law’s help for it in the future if I use it (non-app user).
Health Information Seeking Behaviour (HISB) refers to How individuals seek information about their health, risks, illnesses, and health-protective behaviors (Lambert & Loiselle, 2007; Mills & Todorova, 2016) [29, 30].
Health-related information seekers and chronic diabetics were better at testing their blood glucose regularly and managing diabetes. Surprisingly, individuals irrespective of age, gender, and marital status, with higher income, were associated with online health-related information-seeking behaviors.
P4- Yes, I searched Google and looked for what diet to eat, and hence I have adopted a vegetarian diet. And my brother taught me about doing an online search a year back. Now I google search myself.
T2DM individuals preferred using online platforms like Google search engine to get a deeper insight into the disease and its management. The use of Google search was helpful for 4 participants mainly in planning and managing their diet, practicing mild exercises like walking, and getting prepared to control diabetes complications. Learning and understanding diabetes, not only through online platforms but also through personal experiences from friend groups and newspapers was found to be effective among one of the participants.
Also, a few read articles in the newspaper on the health and wellness sector and found educational TV shows on regional TV channels hosted by physicians useful, to gain an understanding and knowledge of their disease and its management.
Duration of diabetes
The longer the diabetes duration, the more T2DM individuals were confident enough to self-manage diabetes via regular diet, exercise, and blood glucose monitoring as reported by three chronic patients compared to newly diagnosed young T2DM individuals.
P9- I eat more of a veg diet, try to drink sugar-free tea, and walk for half an hour a day.
P3- Now, I am monitoring Glucose four times a day and recording. Now it’s under control with one week of medication they had given me at the hospital.
The study suggests a potential association between diabetes duration and confidence in self-management. The increased confidence seen by three of the participants suggests greater openness to mHealth adoption especially in tracking blood glucose levels, medication adherence, and improved dietary choices. The inclination towards using an app can also suggest enhanced communication with doctors, as well as helping doctors make better treatment decisions.
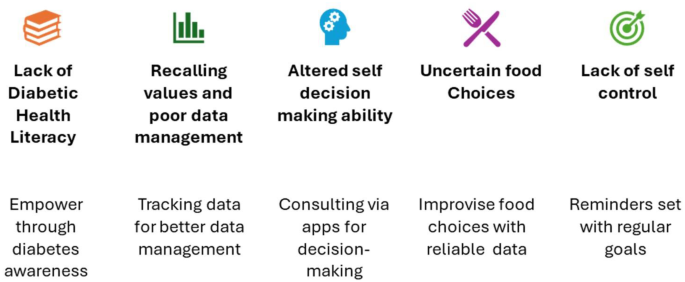
Digital Health Solutions addressed by the researcher according to the patient needs identified (refer: Fig. 2)
Lack of diabetic health literacy
Awareness about one’s health condition, in our case scenario, T2DM is a vital aspect of initiating the actual treatment for improving health outcomes. In this study, the newly diagnosed T2DM Patients were unaware of diabetes, its causes, and symptoms, and ignored the signs of giddiness, fainting, shivering, and feeling thirsty often, unless they got diagnosed in the hospital.
The interviews conducted among patients with T2DM, who were aged 60 and above/chronic diabetics, and especially those who retired from their jobs monitored their blood sugars promptly. They gathered all the information on diabetes for years from their family, and friends and developed a good rapport with their healthcare providers. Whereas the rest of the newly diagnosed T2DM individuals were trying to figure out what was the reason for them to develop diabetes. On being newly diagnosed patients, being asked how they manage diabetes on their own? The participants were found to have problems recalling the health education they were given on managing diabetes by their providers on their first visit.
P3- At the hospital, they told me- it’s late to treat! What can I do? The problem was that in the mornings my blood sugar was low but in the evening my blood sugar levels were high.
Solutions
One way to address the issue of people with poor diabetic health literacy is to launch a public health initiative, such as creating and distributing diabetes education materials. Another technology-driven way is to provide easy-to-access educational materials via Digital Health apps is helpful in this technological age and provide information on the causes and risk factors of diabetes, healthy eating, weight control, blood sugar monitoring and control, medication administration, etc. Diabetes-related health education via an app can be easily accessible anytime and anywhere. This also can help reduce recall issues from the patient’s first doctor visit and recollect the information on diabetes and management leading to enhanced and elevated DSM levels.
Problems with recalling and poor data management
The interviews we conducted among the T2DM patients highlighted poor data management of their health-related data, especially regular blood glucose monitoring, insulin dosage, or medication intake. Two of the chronic diabetic patients interviewed stated that they kept a record of their blood glucose regularly and used reminders for their next visits. But whereas the newly diagnosed diabetic patients were clueless about how to go about tracking and monitoring their health condition.
P2- I keep track of blood sugars once every month by writing on a paper.
P9- I check blood sugar weekly 4 times. I have a blood sugar monitor at home and write it down in the paper that they have given me from the hospital.
Solutions
The mHealth interventions like mobile applications in this situation can help track daily activities and record them to prevent forgetfulness related to age and workload and fear of the paper getting lost.
Incorporating features in the app like reminders for tracking patient medications, blood glucose levels, information on controlling diet, regular exercise, and follow-up hospital visits will be a favorable option to self-manage one’s diabetes condition. Similarly, some of the supporting articles explain a few of the benefits [31, 32].
Diabetes management also involves tracking various data points such as the patient’s daily activities like exercise or weight could be effective in determining the prognosis of the disease [33]. Few patients were also expressive about using their phones for keeping reminders and managing diabetes in their daily lives [34].
Altered self-decision-making ability to manage diabetes
Avoiding confusion on what to do? when the blood glucose readings peak is often a concern among the interviewees as reported by them. They have reported to be trembling and confused about what to decide on their next blood glucose reading.
The need was to know the right dose of medications and methods to follow when their sugar levels peaked or dropped.
P3- As per doc orders I take medicine regularly. But confused
P2- I monitor usually but sometimes I can’t correctly see, so I need to use a lot of time and spend money on extra strips and needles. So, I don’t check often.
Solutions
Blood glucose levels typically peak 1–2 h after eating, depending on various factors like food composition and individual metabolism. Making the patients knowledgeable about their normal blood glucose ranges and preparing them for any emergency is crucial. Hence sharing this information using an app with updated and evident information will enable them to prevent their situation from worsening. Nevertheless, consulting their doctor or healthcare provider on call for personalized guidance is much more beneficial, hence contact information of the treating physician for crucial decision-making at this point will be helpful.
This can keep the patients prepared by knowing their target range, having readily available snacks or medications in hand, and understanding what actions to take based on their reading.
Uncertain food choices
T2DM patients expressing their doubts and lack of clarity about what to eat was another important concern to manage diabetes effectively. Difficulty understanding dietary recommendations can lead to frustration and confusion.
For example, one of the participants in the interview was confused about the diabetic diet and mentioned that she was starving most often because she did not know what to eat. Getting diagnosed with a chronic condition like T2DM can be traumatic and stressful at the same time. Dietary restrictions can add to the burden. Patients might feel overwhelmed, frustrated, or unsure about making healthy choices.
P8- I can’t go without having food, because the doctor advised me to be on a strict diet and eat limited, so I am fasting for a week. I only ate ragi and jowar.
Solutions
The abundance of information available online and from various sources, is often confusing. Patients might struggle to distinguish reliable sources from misinformation. Medical and nutritional terms can be confusing for individuals without a scientific background. Hence including reliable evident information on healthy foods and how to prepare basic recipes is important. Using simple language, visuals, and recipe techniques is necessary with the help of mHealth apps while disseminating health education on diabetes. Active involvement of the HCPs to develop individual meal plans based on their specific needs and preferences is another non-technological solution that could be made technology-dependent with the dietician’s active involvement.
Lack of self-control
Another problem faced by the patients is, to abide by strict monitoring and glucose control due to irregularity in daily activities performed, along with the patient’s inability to maintain a healthy diet for longer. For example, one of the participants stated that they could not resist eating food items that were not healthy and ended up eating higher quantities at a time.
Solutions
Use an activity tracking feature in the mHealth app to track patients’ activity levels, identify patterns, and features to set reminders to continue and motivate the individuals to monitor and self-manage diabetes regularly. This can help adjust patients’ exercise routine or insulin intake based on their activity level on any given day.
The solutions for the problems faced by the patients listed above could be put forth by customizing a mHealth app with all features put together. Accurate and reliable data on diabetes conditions from various standardized national and international organizations like the American Diabetes Association (ADA), International Diabetes Federation (IDF), and the World Health Organization (WHO) at the International levels and national levels Indian Council of Medical Research (ICMR), will work towards the better health of an individual and getting optimum health outcomes. Educating individuals on the core of DSM, avoiding future complications, and early prevention for those individuals whose HbA1c values are just at border levels might help mitigate the future disease burden in India.





Add Comment