Socio-demographic characteristics
In the sample of 408 students, 271(66.4%) were medical students and 137(33.6%) were nursing students. Participants had a mean age of 23.9 (SD = 2.3) among medical students and 24.1 (SD = 2.8) among nursing students. Two hundred (49%) participants were in their final year, while two hundred and eight (51%) participants were in their penultimate year. Moreover, 178(65.4%) of 271 students in the medicine discipline and 94(68.6%) of 137 students in the nursing discipline were male. Around 74% of participants identified as heterosexual and 93.6% of the participants were single. In all disciplines, the majority of participants were Christian 84.8%, and moderately religious 60% (see Table 1).
Interest and acceptability of training
Participants reported a high level of interest in receiving training on sexual healthcare of women who have experienced FGM/C. In all, 336(82.4%) participants indicated they were “very interested”, and 63(15.4%) indicated “interested”. Only 2 out of the 408 participants (0.5%) stated they were “uninterested”, and both were medical students. An additional 7(1.7%) provided a neutral answer. Almost all participants reported that this type of training is acceptable, with only 3 individuals indicating disagreement (2 medical students and 1 nursing student).
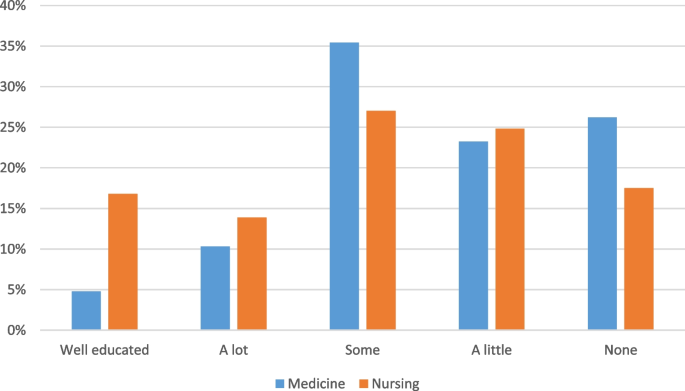
Previous FGM/C training
Participants reported a range of experience in receiving previous training, as indicated in Fig. 1. Most participants did not have a high level of training in sexual healthcare of women with FGM/C – in particular within the medical discipline. Only 16.8% of nursing students and 4.8% of medical students considered themselves well educated.
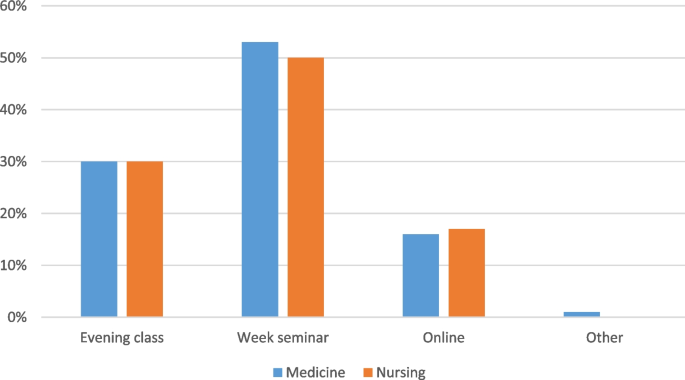
Method of curriculum delivery
Medical and nursing students answered similarly to the method of curriculum delivery they preferred, as demonstrated in Fig. 2. The results indicate a preference for in person training, with about half preferring to have a weeklong seminar held during a typical semester break.
Table 2 shows some differences identified when we compared responses between male and female participants regarding the need for and acceptability of the FGM/C curriculum training for medical and nursing students. Of all male participants, 75% strongly agreed that the curriculum was acceptable, whereas 83% of female participants reported that it would be acceptable for them to receive a curriculum. Most (86.5%) of females and (80%) males were very interested in receiving training on healthcare of women who have undergone FGM/C, with two males reporting to be uninterested to receive the training. Because so few participants indicated a lack of acceptability and interest, we were unable to test for statistical difference between groups.
Thematic analysis
Three themes were identified through the analysis of the open-ended question (1) education to improve competence and confidence, (2) the role and benefits of the training on the impact of FGM/C, and (3) content and approaches for delivering the training. Table 3 shows the summary of qualitative findings, including the codes that were developed into subthemes and finally overarching themes. Notably, there were no codes or themes that indicate any concerns with FGM/C training. Though participants were asked about sexual healthcare, they spoke more broadly to include other types of healthcare such as maternal health and psychological well-being — as will be apparent in the below quotes.
Education to improve the competence and confidence in dealing with FGM/C cases
Participants indicated that training is necessary for improving the competence of healthcare professionals to manage FGM/C related cases. Participants stated they feel a need for more knowledge to better serve patients. For example, many stated they heard of the practice but do not know much about it and have less ability to treat these patients. One participant was quoted saying “With this training I would be able to help in case I encounter patients, friends and family members who outright experience FGM, and if so, offer them directive care for which will be helpful to them.” (Medical student).
Other participants reported lacking confidence when faced with FGM/C patients and hence being unable to help a victim. For example, a medical student stated, “I have seen some women who are victims of FGM, too bad I did not know how to go through, I hope the training would give me the confidence to attend such clients.” (Medical student).
To improve HCPs competence and confidence in handling FGM/C patients, it is also crucial that they are ready for training. The majority of participants stated that training is essential since it is very relevant to society and its applicability will increase as this practice continues in some societies. In addition, they showed interest in learning how to incorporate patient FGM/C information while taking a sexual and medical history. One participant said, “I would like to participate in this training, because it is highly relevant in our society” (Medical student).
Other participants reported “I will be much interested in learning how to take the medical history of a woman with female genital cut.” (Nursing student), “It’s quite important because it’s a major cultural practice in remote areas of our settings.” (Medical student).
Participants demonstrated a desire to join efforts in ending the FGM/C practice. They acknowledged the existence of the practice in society and the need for skills in preventing further impacts as well as a collective effort to combat it. The participants added that the help and support from healthcare professionals is very crucial in addressing the issue. For example, a participant said, “Skills will help in the effort to combat this practice in societies and also help the affected individuals.” (Medical student), and another similarly stated, “This will also contribute to reducing the events of FGM in Tanzanian, societies of Tanzania, particularly in the rural regions.” (Medical student).
Another participant expressed the need of having adequate knowledge for eradication by saying, “We need knowledge to know how we can combat and eradicate female genital cutting in areas where the community have not been educated on disadvantage of female genital cutting” (Medical student).
Role of training on addressing the impact of FGM/C
Participants demonstrated some comprehension of the FGM/C practice and its consequences. They stated that FGM/C is a taboo subject that violates human rights and has resulted in many health impacts, including sexual challenges. Participants asserted that FGM/C can result in emotional and psychological problems and has contributed to marriage instability as a result of sexual health challenges. “Female genital cutting has many negative impacts like tears and excessive bleeding during delivery, which can lead to death, painful sexual intercourse, psychological trauma, and failure to enjoy sex or achieve orgasm. So, the training will help us to gain knowledge and raise community awareness about the effects of this harmful cultural practice as well as help the females who are at risk” (Medical student).
Participants believed that the training would equip them with knowledge necessary to effectively handle FGM/C cases, hence improving their practices. For example, 1 participant remarked that, “It will help me in identifying the sexual heath challenges experienced by women who have undergone female genital cutting and provide the necessary care” (Medical student). In addition, they stated that training would remind HCPs of their role to provide health education to women and to protect their reproductive and sexual health, hence reducing sexual health challenges and enhancing their mental health.
Participants expressed that training HCPs in the health care needs for women with FGM/C would improve the provision of proper childbirth care for these women, hence reducing childbirth complications and saving their lives. “It will help to reduce childbirth complications particularly postpartum haemorrhage, for this specific group, HCPs will be able to care for them and provide them with information about sexual and reproductive health” (Nursing student).
The community benefits of the training were also emphasized, as the training will provide HCPs knowledge needed to educate society about the impacts of FGM/C. For example, HCPs will be able to raise awareness of the effects of FGM/C, minimize the burden of FGM/C related impacts such as infections and sexually transmitted diseases, and eliminate stigma. “It is important to get trained in sexual healthcare for women in regard to FGM because we need to gain a great deal of knowledge about it in order to educate our society/community about the bad impacts of FGM” (Medical student).
Content and approaches for delivering an impactful training on FGM/C
Participants also urged on an emphasis on the training’s content being culturally sensitive. They further noted that it would be beneficial if the training curriculum included evidence-based explanations of why FGM/C is a detrimental practice by focusing on its impacts. In addition, they emphasized the importance of focusing on psychological and emotional assistance as well as how to treat other complications.
“The training has to provide the facts as to why female genital mutilation is harmful, so that clinicians could know how to deal with FGM cases and properly educate the public the consequences”. (Medical student)
The majority of students would prefer that the training involved a greater number of HCPs and to last longer. In addition, they emphasized that, in order to acquire adequate skills, the training methods should involve a practical session, a physical discussion with individuals who have undergone FGM/C who would share their experiences, and/or the use of standardized patients. For instance, 1 student stated,
“This type of teaching might benefit greatly from the use of standardized patients” (Nursing student)





Add Comment