Study objectives
The primary objective of this study is to evaluate the effectiveness and impact of RASP on high-cost health services utilization (e.g. ED visits, mobile crisis visits and inpatient mental health utilization). To achieve this objective, we will conduct a within-subject comparison by analyzing health services utilization data from patients attending the RASP program one year pre- and post-assessment. Additionally, a between-subject comparison will be made using historical data from a control population consisting of patients referred by a PHP to see a mental health clinician before RASP implementation. Another primary objective is to assess qualitative data from healthcare partners’ perceptions related to the impact of the RASP on access to community mental health care for patients and support for primary care providers, as well as to determine patient experiences and satisfaction with the program.
The secondary objectives of this study are to i) identify the sociodemographic characteristics of the population assisted by the RASP, ii) evaluate the prevalence and correlates of the various psychological conditions of the assisted population, iii) assess recovery, well-being, and risk measures in the assisted population at the program entry, and iv) compare health services utilization in the subset of patients who opt to participate in the Text4Support RCT with those who do not.
The study seeks to address the following research questions:
-
A.
Effectiveness and Impact on Health Services Utilization of the RASP:
-
1.
Did RASP increase the volume of patients referred by PHP? Measured by the number of patients referred by a PHP for a psychiatrist consultation before and after RASP implementation.
-
2.
Did RASP increase the proportion of patients triaged by Central Intake services who had direct access to psychiatric consultations? Measured by the proportion of referrals received by central intake that were booked directly for psychiatry consultation, before and after RASP implementation.
-
3.
Did RASP reduce wait times for access to psychiatrists in the publicly funded MHAP? Measured by the number in calendar days waiting from date referral was received by Central Intake to date patient is scheduled for a psychiatric consultation before and after RASP implementation.
-
4.
Did RASP improve efficiency of the Community Mental Health Programs (CMHP) to address the mental health needs of patients with complex mental health needs? Measured by wait-times for assess to psychiatrists within the CMHP following a referral by a mental health clinician before and after RASP implementation.
-
5.
Did RASP reduce the volume of patients referred by PHP to the ED for a psychiatric consultation? Measured by the number of patients referred by a PHP for a psychiatrist consultation at the ED before and after RASP implementation.
-
6.
Did RASP reduce ED visits, mobile crisis visits, and inpatient mental health services utilization? Measured by the number of mental health and addictions (MHA)-specific ED visits, number of mobile crisis visits, number of MHA-specific hospital admissions, and number in calendar days in LOS for Central Zone patients, before and after RASP implementation.
-
7.
Did patients who attended the RASP and opted to participate in the Text4Support RCT differ in their health services utilization compared to patients who opted not to participate in the Text4Support RCT? Measured by the number of MHA-specific ED visits, number of mobile crises calls, number of MHA-specific hospital admissions, and LOS in calendar days, one-year post-RASP assessment.
-
8.
What are the costs and benefits to Nova Scotia Health from having a RASP for mental health? Measured by the net cost savings associated with RASP considering costs associated with the program and costs saved from avoided high-cost health services utilization (ED visits, mobile crisis visits, and inpatient treatments).
-
1.
-
B.
Perspectives and Experiences of Healthcare Partners and Patients
-
1.
What are healthcare partners’ perceptions related to the impact of the RASP on access to community mental health care for patients and support for primary care providers? Measured by qualitative data from key informant interviews with program directors, psychiatrists, primary healthcare providers, MHA service leaders, and representatives from community organizations.
-
2.
What are the patients’ perceptions related to their overall experience and satisfaction with the service received? Measured by quantitative and qualitative data from the RASP’s satisfaction survey and qualitative data from focus group sessions with a sub-group of the assisted population.
-
1.
-
C.
Population Characteristics and Mental Health Measures
-
1.
What proportion of patients seen at the RASP continued their treatment with PHP? Measured by the number of patients fully discharged back into the care of their primary healthcare provider with treatment recommendations (chart review data).
-
2.
What proportion of patients seen at the RASP were referred to a community mental health program? Measured by the number of patients referred to a community mental health program by RASP psychiatrists (chart review data).
-
3.
What proportion of patients seen at RASP needed additional psychiatric evaluation at the RASP? Measured by the number of re-referrals to RASP by a PHP.
-
4.
What are the sociodemographic characteristics of the assisted population at program entry? Measured by the frequency and percentages of the sociodemographic characteristics (e.g. age, sex of birth, gender, ethnicity, employment status, source of income, income range, relationship status, family support, housing status, education, provincial zone) (chart review data).
-
5.
What is the status of patients’ recovery and health quality index, and the prevalence of likely major depressive disorder (MDD), likely generalized anxiety disorder (GAD), low resilience, childhood trauma, substance use, and suicide risk at program entry? Measured by patient-completed validated scales scores (chart review data).
-
6.
What is the prevalence of patients’ diagnoses made by RASP psychiatrists at program entry? Measured by the frequency and percentages of each psychiatry diagnosis after psychiatry assessment (chart review data).
-
7.
What are the risk factors for ED presentation for mental health concerns and inpatient psychiatric treatments? Measured by Odds Ratios using logistic regression models with sociodemographic and clinical data from the assisted population one year before and after RASP assessment date.
-
1.
Hypothesis
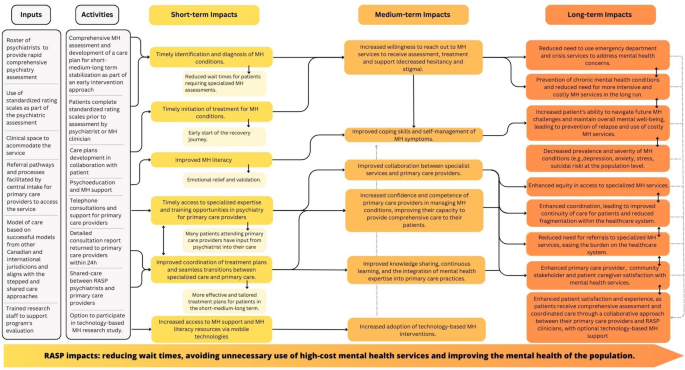
Based on the project Logic Model (Fig. 2), we anticipate that the RASP initiative will yield positive impacts in the short, medium, and long terms, leading to substantial changes in the capacity of mental health support and primary health care providers. Specifically, we hypothesize that RASP will result in a minimum 10% reduction in high-cost health services utilization (e.g. ED visits, mobile crisis visits, and inpatient treatments) and corresponding 10% cost savings. Additionally, we anticipate a reduction in the wait times for patient consultations with psychiatrists within the publicly funded MHAP to less than 30 calendar days. This forecast is expected to be found in both within-subject and between-subject comparisons. In addition, we hypothesize that at least 90% of patients attending the RASP will express satisfaction with the services received. Finally, we hypothesize that primary care providers and healthcare partners will express high satisfaction with RASP. These hypotheses are derived from anecdotal evidence gathered from a similar program implemented at Fort McMurray between 2013 and 2016 by the Senior Investigator.
Study design
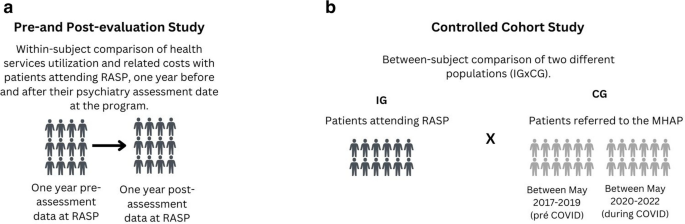
This is a hypothesis-driven program evaluation study that employs a mixed methods approach to evaluate the RASP. It consists of a within-subject comparison (pre- and post-evaluation study) and a controlled between-subject comparison (cohort study). The pre-and post-evaluation study will examine health services utilization data from patients attending RASP, one year before and one year after their psychiatry assessment at the program (Fig. 3a). The pre-and post-evaluation of health services utilization will also enable a comparison between RASP patients who choose to participate in the optional Text4Support RCT and those who choose not to participate in the optional Text4Support RCT.
The cohort study will compare two study populations: the intervention group (IG) consisting of patients attending RASP, and the control group (CG), comprising a cohort of patients who were referred by PHP to the MHAP central intake services prior to RASP implementation (Fig. 3b). This design allows researchers to examine whether possible changes in high-cost health services utilization are associated with the intervention (RASP).
A cross-sectional evaluation of mental health outcomes at program entry will be employed to evaluate the prevalence and correlates of the various psychological conditions of the assisted population.
Patient experience and satisfaction will be assessed using both quantitative and qualitative data. The quantitative data will be extracted from the program’s satisfaction survey, while the qualitative data will be gathered from a purposive sub-sample of the overall study population. The selected sub-sample will be invited to participate in focus group discussions as part of a sub-study to gain deeper insights into their experiences and perspectives. Key informant interviews will be conducted to obtain qualitative insights from various healthcare partners, including directors, psychiatrists, primary healthcare providers, MHA service leaders, and community organizations. These interviews will focus on their perceptions regarding the impact of RASP on patients’ access to community mental health care and the support it provides for primary care providers. Qualitative descriptive methodology and thematic analysis will be employed to generate and refine the information and identify patterns or themes within the qualitative data [35, 36]. This research protocol has been approved by the Research Ethics Board at Nova Scotia Health (REB file #1028254). The Gantt chart timeline is presented in the supplementary material (Table S1).
Participants and data collection
All RASP patients receive a consent form as part of their intake process, allowing access to their health services utilization records. Only those who sign the consent form will be part of the study. While consent is obtained during the initial assessment for ongoing patient recruitment, data collection is scheduled to commence after the program’s first year, in April 2024. Service utilization data will extracted from provincial information systems retrospectively and prospectively at 2-time points: one year pre- and one-year post-assessment date at RASP. In addition, sociodemographic and mental health assessment information, including results from patient-completed validated scales and psychiatry diagnosis, and patient satisfaction will be extracted from routine paper-based initial screening forms. Patient satisfaction quantitative data will be extracted from RASP’s patient satisfaction survey, available in a paper-based format and completed immediately after the assessment or REDCap online survey link sent via text message to all patients attending the service just after the assessment appointment.
The control group for the cohort study will comprise patients referred to the MHAP Central Intake Services by a PHP before RASP implementation. The periods for inclusion in the control group will be May 2017 to May 2019 (pre-COVID) and May 2020 to May 2022 (during COVID). By examining the data from these two time points (pre-COVID and during COVID) and comparing them with each other and with data during the RASP implementation period, we will be able to evaluate the impact of the pandemic on health services utilization as well as the impact of RASP implementation in comparison with both the pre-pandemic and during the pandemic periods. Ethics approval for exemption from requiring informed consent for all control group patients has been granted by the Research Ethics Board at Nova Scotia Health (REB file #1028254), allowing control group patients’ sociodemographic and health services utilization information from provincial administrative databases to be accessed by the investigators.
For the qualitative component of the study, expected to take place after a year of RASP implementation, in April 2024, a sub-sample from the overall pool of the intervention population (RASP patients) will be invited by a research team member to participate in a focus group session. The inclusion criteria to participate in the qualitative sub-study are to provide consent and be available to attend a 1-hour focus group session, which will be audio-recorded. The focus group script will be developed by investigators, reviewed by healthcare partners, piloted with patients and adjusted as needed, before being used in the focus groups. A trained research team member will conduct the encounters, which may happen in person or via Zoom. The sample size for the qualitative component of the study cannot be predetermined because data saturation needs to be reached. Data analysis ends when no new themes and subthemes emerge across all analysts. However, based on what the literature suggests [37], we anticipate that 25-30 participants may be sufficient for this mixed-methods study. Participants will receive compensation for their time spent participating in the qualitative sub-study activities.
Healthcare partners involved with RASP will be also actively engaged in the qualitative evaluation of the program. Trained members of the research team will conduct individual key informant interviews, either virtually or in person, with program directors, psychiatrists, primary healthcare providers, MHA service leaders, and representatives from community organizations. These interviews aim to gather in-depth information about healthcare partners’ experiences and opinions regarding the program, allowing for a comprehensive understanding of their perspectives.
Finally, a sub-population of RASP patients who opted to participate in the Text4Support RCT will also have their one-year pre- and post-RASP attendance health services utilization data collected and compared to patients who chose not to participate in the optional Text4Support RCT. RASP was launched in April 2023, with data collection ongoing. Table S2 demonstrates in detail the variables, sources and data collection time points.
Outcome measures
Primary outcome measures will include the mean differences in the frequency/duration/related costs of high-cost mental health services utilization (i.e., volume and proportion of mobile crisis visits, ED visits, hospital admissions and readmissions and associated LOS for each admission) between one year pre- and post-assessment date for same patients at RASP (within-subject comparison) and between the IG (RASP) and CG (historical data) (between-subjects comparison). Other primary outcome measures will be the mean difference in the number and proportion of total referrals booked directly for a psychiatrist and the number of calendar days for access to psychiatrists, also compared to the control group.
Secondary outcome measures include the mean difference in the frequency/duration/related costs of high-cost health services utilization one year post for patients who access the RASP and participate in the Text4Support RCT (to receive either daily supportive text messages or a single text message with a link to e-mental health resources) and patients accessing RASP but who do not participate in the Text4Support RCT. Other secondary outcome measures include a descriptive summary of the sociodemographic and clinical characteristics of the assisted population, the mean scores on the Patient Health Questionnaire 9 (PHQ-9) [38], Generalized Anxiety Disorder 7 (GAD-7) [39], World Health Organization 5 (WHO 5 Well-Being Index) [40], Brief Resilience Scale (BRS) [41], Recovery Assessment Scale (RAS) [42], Adverse Childhood Experience (ACE questionnaire) [43], Brief Substance use Craving Scale (BSCS) [44], and the Columbia-suicide severity rating scale (C-SSRS) [45], as well as the prevalence of likely MDD, GAD and low resilience. Patient overall impressions (i.e. barriers to accessing RASP, satisfaction level, likely recommend the service to others, etc.) and impressions on the experience (i.e. feelings of welcomeness, respect, enough time to talk, the problem addressed, and understanding of treatment) are part of the patient satisfaction quantitative evaluation. An in-depth evaluation of healthcare partner impressions and patient satisfaction will be obtained through qualitative key informant interviews until saturation is reached and no new themes and subthemes emerge.
Sample size considerations
With two staff psychiatrists and a clinical coordinator, we expect an average of six patients to receive comprehensive psychiatric assessments at the RASP each working day. Thus, we anticipate that the total number of patients accessing the service over the 24-month data collection period would be at least 2500. We also expect the sample size for the control population (patients whom a primary care provider referred to the MHAP Central Intake Services between May 2020 and May 2022) to be at least equal to the numbers seen at the RASP over a similar two-year time frame. Therefore, the data set to be generated from an overall sample of 5000 patients in this study would be large. With the assumption that the implementation of RASP will lead to at least a 10% reduction in high-cost health services utilization one-year post initial referral from a primary care provider for patients attending the service compared to patients who were offered a future appointment to see a mental health clinician as an entry point to the community mental health program, a power of 90% (β = 0.1) and a two-sided significance level of α = 0.05, and assuming an aggregated mean high cost health services utilization of 10 (SD =1) for the control population, we estimated that a sample size of 525 per group would be sufficient. Given that we expect at least 2500 patients per group in our study, it is highly probable that our study has more than sufficient power to detect the projected differences in high-intensity/cost health services utilization between the two groups.
Data analysis
Quantitative analysis
Quantitative data will be analyzed using descriptive and inferential statistics by using SPSS version 26 for Windows [46]. First, we will summarize the study participants’ sociodemographic and clinical descriptive characteristics. Primary outcomes comparing the pre-and post-enrollment health services utilization for patients accessing RASP will be analyzed using descriptive and inferential statistical analysis, including Chi-Square and independent sample t-tests. For the primary outcome involving control populations, pre- and post-enrollment health services utilization variables will initially be compared using an analysis of covariance (ANCOVA) with the intervention condition (attended RASP) as the independent variable, the relevant health services utilization data one year pre attendance of appointment with RASP psychiatrist or community mental clinician as the covariate, and the relevant high-cost health services utilization data one year post attendance of appointment with a RASP psychiatrist or attendance with mental health clinicians in the community mental health program as the dependent variable. In each case, checks would be conducted to ensure no violation of regression slopes and reliable measurement of the covariate. We will perform sensitivity analyses of covariance to explore the impact of the imputation of data loss at each time point on health services utilization. In addition, we will perform propensity score matching and regression analyses adjusting for the periods pre-, during and post COVID-19 pandemic in order to strengthen the comparability of the groups and enhance the validity of the study’s findings.
We will also use an ANCOVA to compare high-cost health services utilization data for one-year pre- and post-RASP attendance for the subset of patients who attend RASP and either participate or do not participate in the Text4Support RCT. For this analysis, the intervention condition (participants in the Text4Support RCT) will be the independent variable, the relevant health services utilization data one-year pre-attendance of appointment with RASP psychiatrist will be the covariate, and the relevant high-cost health services utilization data one-year post attendance of appointment with a RASP psychiatrist will be the dependent variable.
Using data from the first preliminary data analysis at the end of Year 2 and refining this at each subsequent analysis, we will perform regression to predict characteristics and risk factors for ED presentations for mental health concerns and inpatient psychiatric treatments [47]. For the categorical primary outcome measures, we will use the Chi-square test and multivariate logistic regression analysis to explore predictor variables for high-cost health services utilization variables of interest.
Health economic evaluation
We will conduct an economic evaluation through an effectiveness-implementation science lens. Specifically, we will conduct a cost-consequence analysis (CCA) from a Canadian single-payer perspective. The CCA will involve a disaggregated comparison of the costs and benefits (consequences) associated with RASP. The disaggregated analysis reports the intervention effects for the relevant primary and secondary outcomes in their natural units to aid value for money assessments. The study design, population, setting, and location are described elsewhere in this proposal.
We will compare outcomes (ED visits, crisis calls and inpatient days) and costs in the intervention group to the control group. Costing includes costs associated with the pre-implementation, implementation, and ongoing costs. These costs will include space and utilities, new hires specific to RASP, supplies, materials, and equipment, travel costs, volunteer time, and other in-kind donations. We will exclude all research-related costs. These cost data will come from the project documents. In addition, we will collect cost data on health resource use from the case costing centre in the Nova Scotia Health, supplemented with data from the literature if necessary.
Costing will also include costs saved from avoided ED visits, crisis response services and inpatient treatments. Cost analyses will use Nova Scotia Health 2023 costs to ensure relevance to decision-makers. We will estimate the intervention effect for the outcomes using appropriate treatment-effect econometric models with bootstrapping to quantify the uncertainty around the estimates. To enable cost comparisons, the cost of the current models of community-based mental health services, which involve waitlisting of all non-urgent patients (regardless of referral source and reason for referral) to see a mental health clinician as a gateway to receipt of community mental health services, including psychiatry, will be compared with the costs of alternative treatments offered expeditiously through RASP and primary care and community providers. We will compute the net cost savings associated with RASP. Our economic analysis will follow guidelines for economic evaluations, including using probabilistic sensitivity analysis to quantify the uncertainty around the implementation costs [48].
Qualitative analysis
Aligned with qualitative descriptive methods, the qualitative data analysis will be guided by the six-phase thematic analysis framework [36]. We will transcribe verbatim all audio records from the semi-structured individual interviews and focus groups and enter them in NVIVO 12 [49] software for data organization and preparation for analysis.
The first step of qualitative analysis is to become familiar with the data, reading and re-reading the transcripts. At this stage, we will also perform data validation for quality assurance purposes. A data validator, who is a separate individual from the transcriber, will compare the verbatim transcriptions with the recorded interviews for verbal and non-verbal errors (commissions and omissions). After that, the subsequent phases of thematic analysis (coding, searching for themes, themes review, themes definitions, and writing) will be completed [36]. As previously mentioned, the sample size for the qualitative sub-study will depend on data saturation [37].





Add Comment