Patients and study design
This was a single arm trial at the Obstetrics and Gynecology Hospital of Fudan University, China. The eligibility criteria for ESLS included stage II to IV apical prolapse with previous total/subtotal hysterectomy. All women who met the above criteria between January 2020 and May 2021 were included in this study. The study was approved by our institutional review board (2019-32). All patients gave written informed consent for the surgical procedure and for the use of individual data for research.
The following parameters were included: patient demographics, perioperative outcomes, and short-term results (Pelvic Organ Prolapse Quantification (POP-Q) scores to assess physical prolapse; Pelvic Floor Distress Inventory-20 (PFDI-20) to assess quality of life; mesh exposure and prolapse recurrence). The perioperative data included operative time (from anesthesia to the end of surgery, including other concurrent surgeries), estimated blood loss, surgical complications (injury, blood transfusion, pain, hematoma, infection, and any other complications attributable to the procedure), and recovery of normal diet after operation. Pain was assessed at postoperative 24 h using the visual analog scale (VAS) score: from 0 = no pain to 10 = worst pain. Postoperative follow-up visits were scheduled at 1, 3, 6, and 12 months after surgery.
The POP-Q scores and physical examination were assessed before surgery and at each appointment. Mesh exposure was defined as any mesh that was visible in the vagina on physical examination [6]. Prolapse recurrence was defined as (1) any POP-Q ≥ stage II and (2) any retreatment (pessary or surgery) for prolapse [7].
The PFDI-20 was collected before surgery and at 12 months after surgery. The PFDI-20 includes 3 scales, including the Pelvic Organ Prolapse Distress Inventory 6 (POPDI-6), Urinary Distress Inventory 6 (UDI-6) and Colorectal-Anal Distress Inventory 8 (CRADI-8), with higher total scores indicating a more severe impact of pelvic organ prolapse on quality of life.
Surgical procedures
All operations were performed by the same medical team who specialized in pelvic floor reconstruction surgery and vaginal surgery and had rich experience in vNOTES in our hospital. The videos showed the surgical techniques. The day before the surgery, the patients received vaginal irrigation without intestinal preparation (such as by drinking laxatives or via an enema to empty the intestinal canal). Prophylactic antibiotics (cefuroxime) were administered 30 min before the surgery. The patient was placed in a lithotomy position to allow exposure for the transvaginal procedure. General anesthesia was performed via endotracheal intubation. A 14 F bladder catheter was inserted to decompress the bladder. In the surgery, a standard rigid 30-degree, 10-mm 3D laparoscope, a single-port device with four trocars (HTKD Med), and 5-mm laparoscopic instruments, including grasping forceps, a needle holder, and an ultrasonic knife (Harmonic), were used.
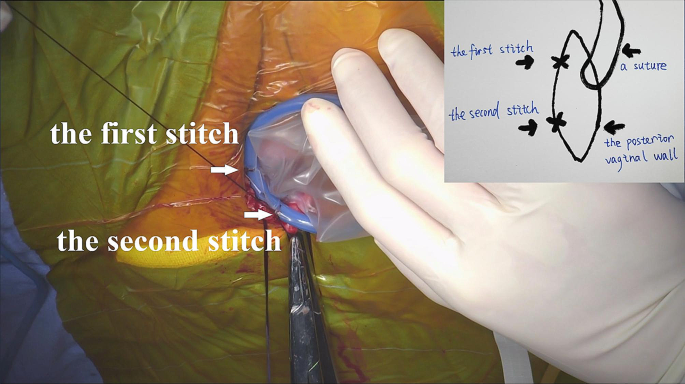
For patients with previous subtotal hysterectomy, transvaginal cervical stump resection was first performed. After an injection of methylene blue into the posterior vaginal wall, a 2-cm longitudinal incision was made. The right lateral rectovaginal space was separated with a monopole electric knife through the wound. A transvaginal single-port platform was established. In contrast to conventional vNOTES, the single-port device needs to be sutured to the vaginal wall (Fig. 1). Additionally, a handmade vaginal retractor cut from an oval negative pressure suction ball was used to hold the single-port device.
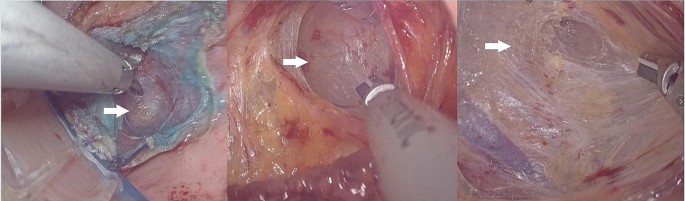
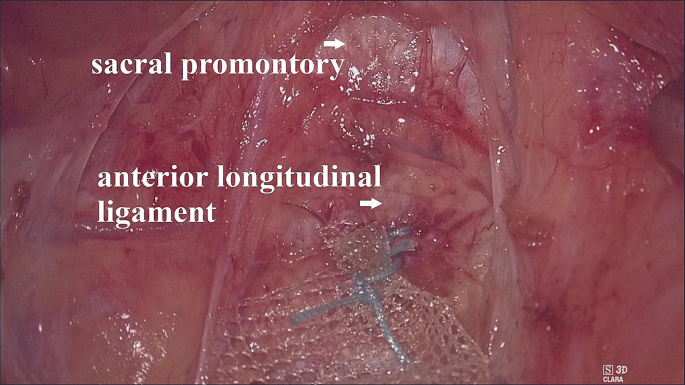
The operating table was first adjusted to a position where the patient’s head was low and the patient’s feet were high; then the operating table was adjusted to lean left. The CO2 pressure was maintained at 16–18 mmHg. When the ‘cotton candy like tissue’ appeared (Fig. 2), we began to establish the retroperitoneal tunnel. First, the ‘cotton candy like tissue’, actually the retroperitoneal fat or loose connective tissue, was separated upward to the sacral promontory with an ultrasonic knife. In this process, we have to be concerned about the right hypogastric nerve (rHN), right iliac vessels, right ureter, and presacral vessels. After reaching the sacral promontory, a mesh (TiLOOP® Mesh, 6,000,486, pfm medical, Germany) was fixed to the anterior longitudinal ligament on the surface of the first sacral vertebra (S1) with a nonabsorbable suture (Fig. 3). The single-port device was then removed. The mesh was hand sutured to the anterior vaginal wall to suspend the vaginal vault. Before suturing, we measure the length of the vagina assuming the vagina vault is restored, and then tailor the mesh according to the length.
After surgery, cefuroxime was administered once. The normal diet was restored on postoperative day 1. All patients were then followed clinically.
Statistical analysis
Data collection and statistical analyses were performed using IBM SPSS Statistics 24.0 software (IBM Corp., Armonk, New York, USA). All variables are presented as the mean and standard deviation (SD) or n and percentage (%). Continuous variables were compared by Student’s t test. A P value < 0.05 was considered statistically significant.



Add Comment