First pregnancy
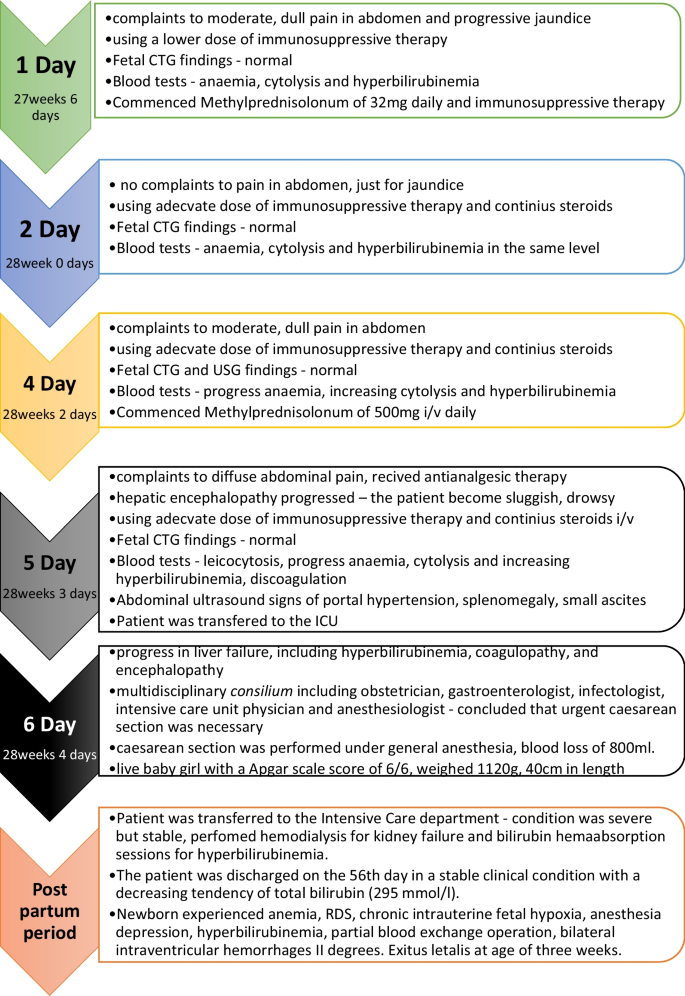
A 19-year-old European patient was transferred to our hospital at 27 weeks 6 days of her first pregnancy owing to her health condition deterioration. She was married, worked in a safe environment, and denied any harmful habits. Contraception was through the use of condoms. There were no chronic or oncological diseases in her family history. She was transferred from a regional hospital to a tertiary hospital owing to complaints of moderate, dull pain in her abdomen, mainly in the right upper quadrant, and progressive jaundice. However, fetal movements were felt to be good. It was noted that she had been using a lower dose of immunosuppressive therapy than had been prescribed and recommended by gastroenterologists.
According to the patient’s medical history, she received a domino-type liver transplant of the right lobe due to autoimmune, hepatitis-induced cirrhosis 5 years previously. Unfortunately, she was not adherent to immunosuppressive therapy, which caused a relapse of autoimmune hepatitis in the graft with a subsequent hospitalization with high cytolysis and hyperbilirubinemia (221 μmol/L) 1 year previously. Methylprednisolone pulse therapy (1000 mg intravenously for 3 consecutive days) was prescribed, which had a positive therapeutic effect. The patient was strongly advised to follow immunosuppressive medication, and possible consequences of nonadherence were explained. During the following 10 months, her liver function tests were almost within the normal range. However, after 11 months, the patient experienced unexpected pregnancy and decided to continue the pregnancy. At week 12, her blood, liver function tests, and tacrolimus trough level were within normal range when reviewed by a gastroenterologist during an outpatient visit. The patient was informed of the risks of immunosuppressive therapy nonadherence as well as explained that the pregnancy was considered high risk. She was recommended to strictly follow the immunosuppressive therapy regimen consisting of tacrolimus, azathioprine (if regular tacrolimus trough level), and liver function test control. The patient had a scheduled follow-up visit with blood analysis 1 month later. Unfortunately, she did not attend subsequent outpatient control visits.
Upon admission to the hospital, the patient took tacrolimus, azathioprine, ursodeoxycholic acid, and vitamin D with calcium supplements irregularly.
On physical examination, the patient appeared to be conscious, active, and adequately responsive. The skin and mucous membranes were slightly icteric. She was hemodynamically stable with normal respiration function. The abdomen was soft to palpation but diffusely sensitive. There were no signs of peritoneal irritation, and urination was reported as unhindered but slightly darker in color.
The fetal heart rate was measured at 146 beats per minute and rhythmic, with healthy amniotic fluid and the uterus normotonic.
On the third day, fetal ultrasound was performed that showed the fetus’ size corresponded to the 28th week 2 days, with the head recumbent. The fetal heart rate was 143 beats per minute and rhythmic, and amniotic fluid was normal. The placenta was placed high on the anterior wall, and the cervix was closed and 43 mm long.
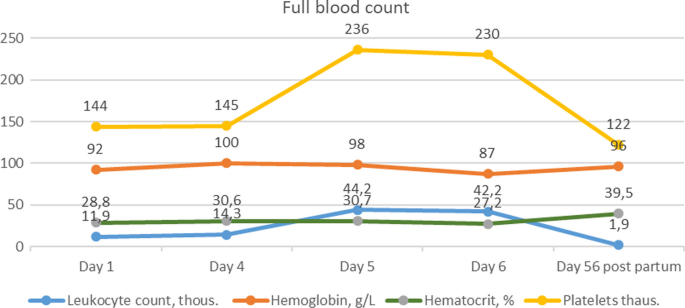
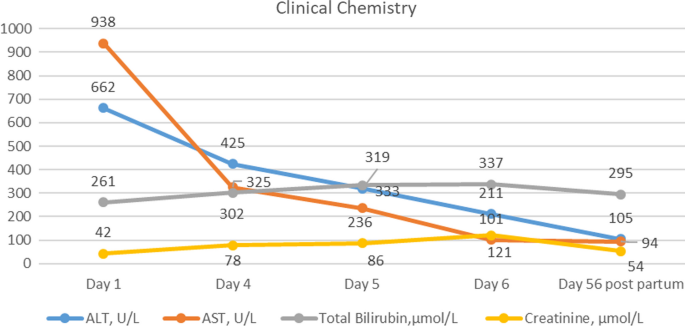
Peroral therapy with methylprednisolonum of 32 mg daily was commenced. On the fourth day of hospitalization, additional 500 mg of methylprednisolone was administered intravenously for three consecutive owing to increasing cytolysis. On the fifth day of admission, the patient experienced diffuse abdominal pain, which was treated with antianalgesic therapy. Abdominal ultrasound revealed signs of portal hypertension, including splenomegaly, portal vein dilatation, small ascites, and mild (grade 1) bilateral urostasis associated with advanced pregnancy. However, the patient’s condition worsened and hepatic encephalopathy progressed—the patient became sluggish and drowsy. On the sixth day, due to hepatic encephalopathy progression (Figs. 1,2), the patient was transferred to the intensive care unit (ICU).
On the morning of the sixth day, a multidisciplinary concilium including an obstetrician, gastroenterologist, infectologist, intensive care unit physician, and anesthesiologist concluded that urgent caesarean section was necessary owing to the rapid deterioration of the patient’s liver failure, including hyperbilirubinemia, coagulopathy (Table 1), and encephalopathy. The operation was considered to be high risk owing to the patient’s general condition and required prepreparation with blood components. At 27/28 weeks, the fetus was viable, but further development could not be predicted owing to the mother’s high hyperbilirubinemia and potential fetal brain damage.
On the same day, a lower laparotomy caesarean section was performed under general anesthesia, resulting in the birth of a live baby girl with Apgar scale score of 6/6. The newborn weighed 1120 g and measured 40 cm in length, 23 cm in chest circumference, and 27 cm in head circumference. The placenta separated spontaneously, weighing 405 g, with blood loss of 800 ml. After the operation, the patient was transferred to the intensive care department (Fig. 3).
The newborn experienced irregular breathing after birth and received respiratory support, requiring both positive end-expiratory pressure (PEEP) and assisted ventilation. Owing to planned surfactant administration, the child was intubated and transferred to the ICU. Enteral feeding through a gastric tube with an adaptive mixture was started on the second day of birth, and the child exhibited adequate diuresis. A Passy Muir valve (PMV), phototherapy, and a partial blood transfusion exchange operation (100 ml/kg filtered, absorbed erythrocyte mass with plasma transfusion to exchange 100 ml/kg circulating newborn blood, performed in newborns with hemolytic disease to reduce hiperbilirubinemia, antibodies of erythrocytes, and sensitized erythrocytes) were administered. On the third day, sedation with fentanyl 2 mcg/kg/hour was given with hemodynamics and adequate diuresis. However, fluctuating oxygen saturation and a heart murmur were detected, along with a large patent ductus arteriosus (PDA) in echocardiography.
The child also experienced anemia. Ultimately, the child was diagnosed with respiratory distress syndrome (RDS), chronic intrauterine fetal hypoxia, anesthesia depression, hyperbilirubinemia, bilateral intraventricular grade II hemorrhages, and anemia on the eighth day. The child was transferred to a children’s hospital, but sadly passed away at the age of 3 weeks.
Postpartum period
During the postpartum period, the patient’s condition was severe but stable after undergoing hemodialysis for kidney failure and two bilirubin hemoadsorption sessions for hyperbilirubinemia in the cardioresuscitation unit. On the sixth day after the cesarean section, the patient was transferred to the gastroenterology department. Immunosuppressive therapy with tacrolimus, azathioprine, and methylprednisolonum 32 mg/day was continued. On the eighth day, a liver biopsy was performed to determine the morphological status of the liver, revealing liver cirrhosis with the formation of pseudolobules and cirrhotic transformation, relapse of autoimmune hepatitis, and no data on transplant rejection. Although the patient’s condition was clinically stable, hyperbilirubinemia continued to progress (424 µmol/l on day 11) and discoagulation remained increased (INR 1.5). After concilium decision on the 12th day, methylprednisolone pulse therapy was readministered for 3 days. On the 19th day, due to the poor prognosis of the patient’s disease, the multidisciplinary concilium decided to include the patient on the active list for liver transplantation. The patient’s hyperbilirubinemia continued to progress (597 µmol/l on the 25th day), leading to repeated bilirubin hemaabsorption sessions on the 26th, 27th, and 28th days. Viral hepatitis A, B, C, and E were ruled out for the patient.
On the 20th day, the patient’s blood sample showed a positive result for cytomegalovirus DNA (quantitatively 1644 copies/ml). On the 26th day, the viral load increased to 2880 copies/ml. The patient was treated with valganciclovir 900 mg/day orally, based on creatinine clearance. The viral load was negative on the 46th day. The patient also underwent consultation with a neurologist, psychiatrist, and psychologist. The patient was discharged on the 56th day in a stable clinical condition with a decreasing tendency of total bilirubin (295 mmol/l) and INR of 1.18. She continued her care on outpatient basis with the supervision of a family doctor, gastroenterologist, and gynecologist. It was emphasized to the patient that she needed to avoid pregnancy for the next 2–3 years and be adherent to medical therapy.
Second pregnancy
The patient’s second pregnancy occurred 1 year after her first one. At 14 weeks into the pregnancy, the patient was informed of possible complications by a multidisciplinary concilium consisting of a gastroenterologist, infectious disease specialist, gynecologist, and psychotherapist. Despite their recommendation to terminate the pregnancy, the patient opted to continue. Later on, she was admitted to the gastroenterology department of a tertiary hospital for further monitoring and examination.
Tables 2 and 3 present the laboratory tests, ultrasound findings, and medications administered during the second pregnancy at various stages of gestation. During her hospitalization, she received methylprednisolone therapy and continued to take azathioprine, tacrolimus, and ursodeoxycholic acid. The patient had an elective caesarean section at 37 weeks owing to a scar on uterus from a previous caesarean section and patient preference. RDS prophylaxis was administered before the procedure, and the baby girl was born weighing 2860 g and measuring 50 cm with 7/8 points on the Apgar scale score. Blood loss during childbirth was 1170 ml, and the patient required two erythrocyte mass transfusions for anemia in the postpartum period. On the fourth day after the caesarean section, the patient and child were discharged in a generally satisfactory condition and referred to outpatient care with a family doctor, gynecologist, and gastroenterologist.






Add Comment