The human immunodeficiency virus (HIV) has infected 38.4 million (33.9–43.8 million) people around the world. In fact, although infection rates have decreased slightly, it is still a major global public health problem with over 1.5 million new infections annually, which led to the deaths of approximately 650,000 individuals in 2021. African regions account for two-thirds (25.6 million) of people living with HIV (PLWH). Eastern Europe and Central Asia represent the cradle of a growing HIV epidemic, and <3% of PLWH live in Western and Central Europe (UNAIDS Report, 2022). In the Moroccan context, the prevalence of HIV-1 in the general population is less than 0.1%, with 22,000 (19,000–24,000) PLWH (PNLS, 2021). The most prevalent HIV-1 subtype is European subtype B, followed by circulating recombinant forms, such as CRF02_AG (15%), which originated in sub-Saharan Africa (Akrim et al., 2012). The widespread use of combined highly active antiretroviral therapy (HAART) has been a very exciting advancement in the treatment of PLWH. It maintains viral loads at undetectable basal levels, limits the emergence of viral resistance, and significantly reduces morbidity and mortality rates (Colomer-Lluch et al., 2018). However, some of the main factors that lead to the failure of HAART arethe development of drug resistance (Murphy et al., 2001; Clavel and Hance, 2016), failure of the host patient’s immune system, poor adherence to treatment regimens, drug toxicity (Ekstrand et al., 2011) and poor multidisciplinary management of PLWH (D’amato et al., 1998), particularly in low and middle-income countries (Hailu et al., 2018).
It is well established that the genetic backgrounds of the host and the pathogen are crucial factors influencing susceptibility to and protection against infectious agents (Qaisar et al., 2020). Several host factors affect HIV-1/AIDS pathogenesis. Chemokine receptor 5 (CCR-5), once truncated, protects against HIV infection by preventing the HIV virion from binding with the host cell. Tripartite motif 5α (TRIM5α), dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin (DC-SIGN), SAM-domain HD domain-containing protein (SAMHD1),tetherin and apolipo protein B mRNA editing enzyme catalytic polypeptide-like 3G (APOBEC3G) (Naranbhai and Carrington, 2017; Ghimire, Rai and Gaur, 2018; Iqbal et al., 2018; Vanessa D’Urbano, 2018; Qaisar et al., 2020; Pagani et al., 2022) are host factors that are counteracted by HIV viral accessory proteins (Ayinde et al., 2012; Imran et al., 2016).
APOBEC3 proteins (A3) have been shown to inhibit the replication of a wide range of exogenousinvading viruses, such as HIV and Hepatitis B virus and endogenous retroelements (Zhang and Webb, 2004; Bishop et al., 2008). Among these, APOBEC3G (A3G; 384 amino acids, 46 kDa) is rated as the most effectiveinnateHIV-1 inhibitor (Sheehy et al., 2002). Yet, in the absence of the viral infectivity factor (vif), a structural part of HIV-1, A3Gis actively packaged into budding HIV-1 virions. Once catalyzed, cytidine-to-uridine mutations in the negative-strand lead to guanine-to-adenine mutations in the proviral DNA during reverse transcription (Sheehy et al., 2002; Goila-Gaur and Strebel, 2008; Giese et al, 2016). The vif of HIV-1, by preserving the viral genomic integrity, neutralizes A3G and related APOBEC3 enzymes (A3D, A3F and A3H). With the transcription cofactor CBF-β, vif heterodimerizes, recruits a Cullin-Ring ubiquitin ligase complex and triggers polyubiquitination of A3 enzymes and their proteasomal degradation after directly binding them (Richards et al., 2017). Despite the presence of vif, A3 enzymes are still able to induce mutagenesis by integrating HIV-1 virions (Mohammadzadeh et al., 2019).
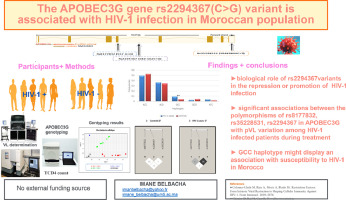
The host’s genetic background can affect viral infections.This includes single-nucleotide polymorphisms (SNPs), and other factors (Ben-ari et al., 2003). Numerous researchers have extensively investigated the genetic polymorphism of A3G in most world populations. However, minimal attention has been paid to African populations. The findings indicate that A3G might have a significant role in the emergence and course of HIV-1, HBV, and HTLV-1 infection (Sasada et al., 2005; Fan et al., 2010).In our study, we analyzed three A3G SNPs namely rs8177832, rs2294367 and rs35228531. Located respectively in exon 4, at intron close to splicing site 162bp (http://snp-nexus.org) and in 3′extragenic region, the A3G variant rs8177832 A>G is known to be involved in the gene expression alteration (Ping et al., 2004); rs2294367 C>G was previously associated with accelerated AIDS progression (Ping et al., 2004); and rs35228531 C>T was reported to be associated with protection against HIV-1 infection in Burkina Faso (Compaore et al, 2016a, 2016b).In accordance with our previous study, neither rs8177832 nor rs35228531showed any association with HIV-1 infection or therapy response (Belbacha et al., 2022).
Thus, the goal of this study was to investigate the genotypic and allelic distribution of the rs8177832, rs35228531 and rs2294367 A3G variants in both Moroccan HIV-1 infected patients and healthy individuals. This was followed by an assessment of their relationship with viral load during treatment and their possible role in susceptibility to the HIV-1 infection.




Add Comment