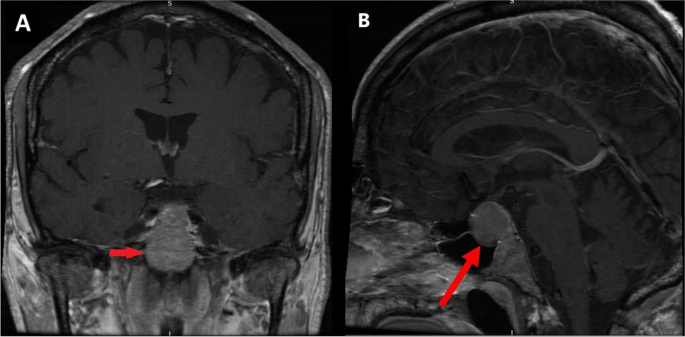
A male patient in his 60s with progressive chronic lymphocytic leukaemia (CLL) despite standard therapy. A combination of ibrutinib and venetoclax have been used in patients with refractory CLL [2] as in this case. His past medical history included trisomy 12 and primary hypothyroidism. A month later he presented to the Emergency Department (ED) with confusion and hyponatraemia. Paired serum and urine sodium and osmolality showed a serum sodium 120 mmol/L, urine sodium 77 mmol/L, serum osmolality 265 mOsm/kg and urine osmolality 792 mOsm/kg. He was diagnosed with Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) and both ibrutinib and venetoclax were stopped during the admission. Hyponatraemia resolved following fluid restriction and both chemotherapy agents were restarted on discharge. Three weeks later, he presented with symptoms of nausea, diarrhoea and hypotension. Bloods again demonstrated hyponatraemia with sodium of 122 mmol/L. A full pituitary profile revealed pituitary insufficiency. Serum 09:00 cortisol was 15 nmol/L with adrenocorticotropic hormone (ACTH) of 11 ng/L. Other blood results included: testosterone 0.42 nmol/L, luteinising hormone (LH) 13 IU/L, follicular stimulating hormone (FSH) 1.7 IU/L, thyroid stimulating hormone (TSH) 0.12 mU/L, thyroxine 12 pmol/L and serum insulin-like growth factor 1 (IGF-1) was normal. Treatment with hydrocortisone was commenced. MRI pituitary revealed a pituitary macroadenoma as shown in Fig. 1. He was discharged feeling “like a new man” on hydrocortisone 15/5/5 mg daily. The haematology team were anxious to stop his treatment and ibrutinib was commenced at a lower dose.
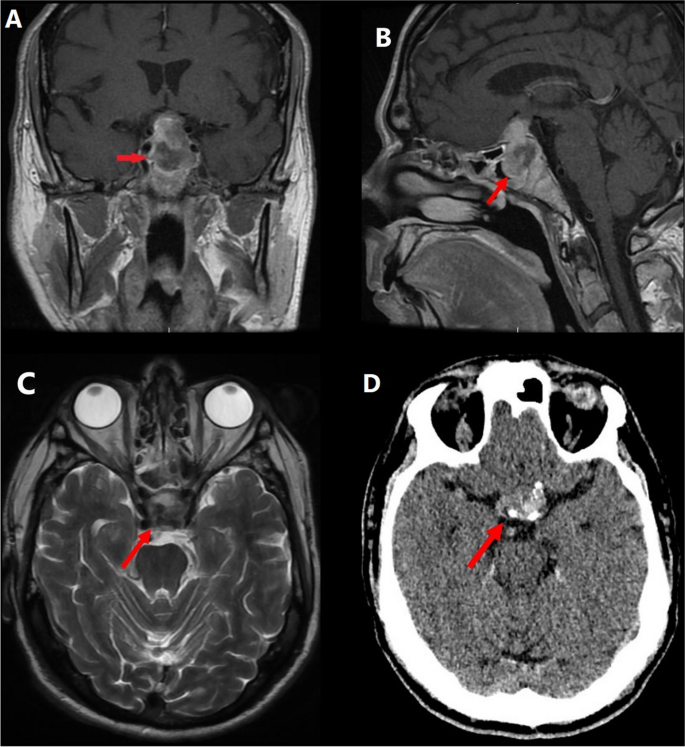
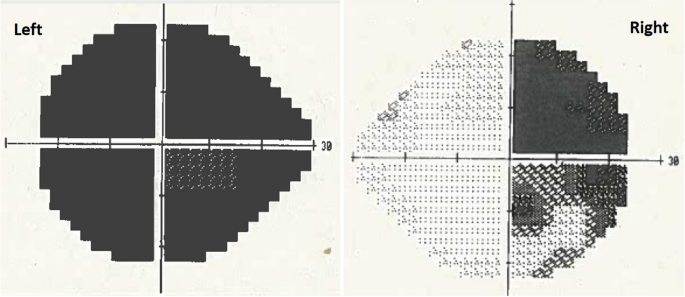
Four months later, the patient presented with a 3-day history of sudden retro-orbital headache associated with vomiting, lethargy and anorexia. Examination findings included left cranial nerve III, IV and XI palsy, left-sided ptosis with blurred vision and diplopia. Left eye examination demonstrated blurred vision and diplopia. Both pupils were mid-dilated and poorly reactive to light; this was more marked on the left. Visual field test by confrontation revealed right temporal hemianopia and near-complete vision loss in the left eye. An urgent CT head followed by an MRI pituitary revealed a 30% increase in the size of the tumour as well as features suggestive of pituitary apoplexy as shown in Fig. 2. The tumour was invading the left cavernous sinus and showed post-contrast unenhanced areas suggestive of necrosis. There was evidence of blood degradation products consistent with a subacute bleed. There was stretching and compression of the optic chiasm. Features were consistent with pituitary apoplexy on an underlying macroadenoma. Humphrey’s visual field examination revealed a left visual field index (VFI) of only 1% with optic disc pallor, while the right was 64% with temporal hemianopia as shown in Fig. 3.
Subsequent imaging 3 months later demonstrating pituitary apoplexy. A T1 coronal MRI showing pituitary macroadenoma (2.6 × 2 × 2.3 cm) with evidence of apoplexy and stretching and compression of the optic chiasm. B T1 sagittal MRI with contrast. C T2 axial MRI without contrast. D non-contrast CT head
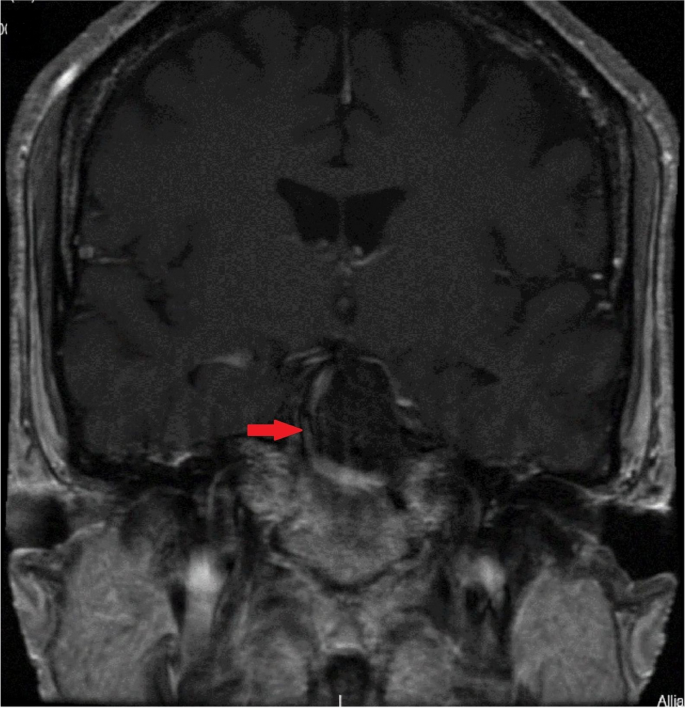
Intravenous hydrocortisone was commenced and the patient urgently referred to the neurosurgical team. He underwent emergency trans-sphenoidal hypophysectomy with circumferential excision of the apoplectic macroadenoma on day seven of the presentation. Follow-up post-hypophysectomy MRI 6 months later showed optic chiasm decompression and a 13-mm residual tumour as shown in Fig. 4.
Post-trans-sphenoidal hypophysectomy, the patient recovered well and had a marked improvement in the right eye and 50% recovery of vision in the left eye. The patient was restarted on ibrutinib and venetoclax 2 weeks following surgery as it was felt that the benefit-to-risk ratio favoured continuation of the treatment and there was little pituitary tissue remaining. The patient had a pituitary MRI at three and 6 months post-operatively which showed a good surgical response.
CLL therapy was withdrawn a year later, following radiological, clinical and biochemical remission. Approximately 1 year post-CLL treatment with ibrutinib and venetoclax, the patient was in complete remission with negative bone marrow for the first time since diagnosis.






Add Comment