Patients
The medical records of patients with bladder cancer who underwent ORC (between September 2015 and June 2021) or RARC/ERAS (between July 2021 and March 2023) at NTT Medical Center Tokyo (Tokyo, Japan) were retrospectively reviewed. Patient characteristics, surgical results, hospital stay, and medical costs were analyzed.
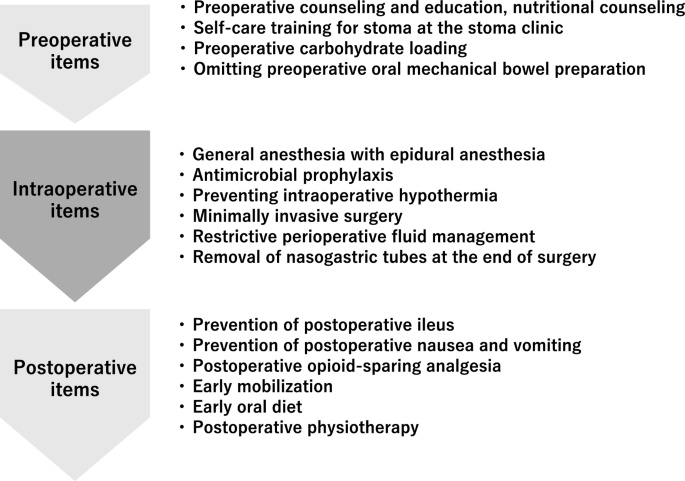
ERAS program
Multidisciplinary ERAS team
Our ERAS items were provided by a multidisciplinary team composed of urologists, anesthesiologists, physical therapists, registered dietitians, nurses, pharmacists, diabetologists, and clinical care pathway committee members as described elsewhere27. The timeline of our ERAS protocol is shown in Fig. 1.
ERAS items
Preoperative items
Preoperative counselling and education and nutritional counseling
Preoperative counseling in the outpatient setting was provided by nationally certified nutritionists, urologists, and anesthesiologists. Patients were advised to maintain a normal diet until the night before surgery unless they had malnutrition according to the European Society for Clinical Nutrition and Metabolism guidelines28. Patients were given a document on their expected recovery after surgery. Preoperative morbidities were optimized as possible.
Patients were taught self-care for stoma at the stoma clinic before the operation.
Preoperative carbohydrate loading
Patients were administered 250 mL of carbohydrate fluid (Arginaid Water®, Nestle healthscience, Tokyo, Japan:100 kcal, 22.5 g carbohydrate with 2.5 g arginine per 125 mL) at 12 and 2 h before surgery.
Preoperative oral mechanical bowel preparation
Oral mechanical bowel preparation was omitted. Sennoside (24 mg) was administered before bedtime on the night before surgery.
Intraoperative items
Anesthesia
General anesthesia was induced using propofol, fentanyl, remifentanil, and rocuronium and maintained using air/oxygen/desflurane, remifentanil, fentanyl, and rocuronium bromide. Epidural anesthesia with 7.5 mg/mL ropivacaine hydrochloride hydrate was provided. The total amount of fentanyl was restricted to 5 μg/kg. Intravenous acetaminophen was administered before the end of surgery.
Preventing intraoperative hypothermia
Warming blankets (Full Body Bair Hugger™, 3 M) were used to prevent hypothermia during surgery.
Minimally invasive surgery
RARC was performed by experienced urologists certified by the Japanese Urological Association using the Da Vinci Xi® system (Intuitive Surgical Ltd., Sunnyvale, CA, USA). Urinary diversion was performed intracorporeally (intracorporeal urinary diversion [ICUD]). The small intestine was cut and anastomosed using the SureForm® stapling system (Intuitive Surgical Ltd., Sunnyvale, CA, USA).
Resection site drainage
A drainage tube (8 mm) was placed at the bottom of the pelvic cavity until postoperative day (POD) 1.
Restrictive perioperative fluid management
Intraoperative intravenous fluid administration was limited to 3 mL/kg/h, and it included Ringer’s bicarbonate solution, antibiotics, and acetaminophen.
Nasogastric intubation
Nasogastric tubes were removed at the end of surgery.
Postoperative items
Urethral drainage
A double-lumen urethral catheter (20 Fr) was placed in the neobladder until its removal on POD 14 in patients who underwent ileum neobladder urinary diversion.
Prevention of postoperative ileus
To prevent postoperative ileus, patients were encouraged to chew gum every 3 h starting 3 h after surgery. Magnesium oxide (300 mg) was administered three times daily until POD 7.
Prevention of postoperative nausea and vomiting
To prevent postoperative nausea and vomiting, 6.6 mg of dexamethasone were intravenously administered at the induction of anesthesia.
Postoperative opioid-sparing analgesia
For postoperative analgesia, patients were intravenously administered 1000 mg of acetaminophen every 6 h for 24 h and oral celecoxib (200 mg) every 12 h.
Early mobilization
The patients were instructed to stand 3 h after surgery. The physical therapist assessed the patients’ condition and assisted with early mobilization from POD 1. On POD 1, patients were encouraged to walk 100 m and attempt to be out of bed for 6 h. They were also encouraged to be out of bed for more than 2 h. On POD 2, patients walked more than 300 m with assistance by physical therapists. They were encouraged to be out of bed for more than 6 h.
Early oral diet
Patients were allowed to drink clear fluid 3 h after surgery. A liquid diet was also provided 3 h after surgery.
Statistical analysis
Fisher’s chi-squared test was used to analyze categorical variables. Mann-Whitney U test was performed to analyze numerical variables. Statistical significance was indicated by P < 0.05. All statistical analyses were performed using SPSS version 24.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki (revised in 2013).
This study is approved by the ethics committee of NTT Medical Center Tokyo. Informed consent was obtained in the form of opt-out on the web-site. Those who rejected were excluded.





Add Comment